Lancet:并非所有的免疫治疗都能创造奇迹——帕博利珠单抗未能延长胃/胃食管结合部癌症患者总生存
2018-06-20 biubiugirl 肿瘤资讯
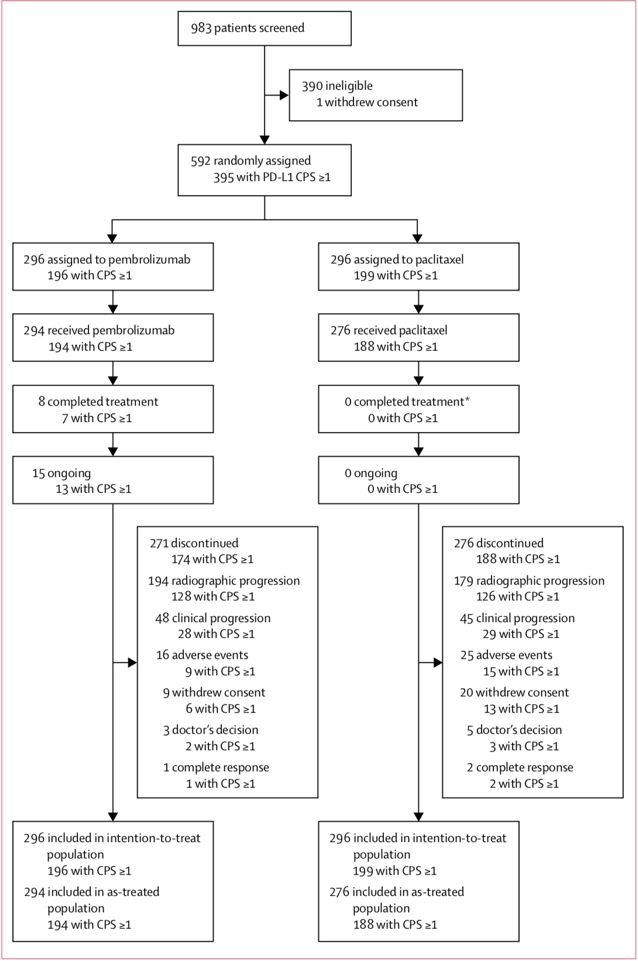
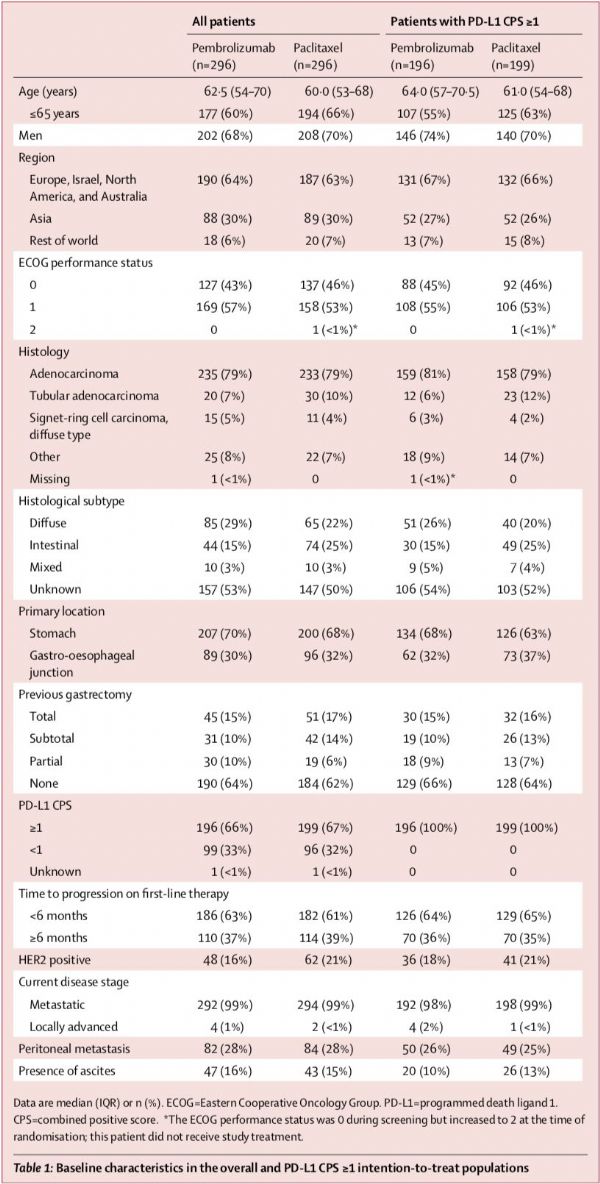
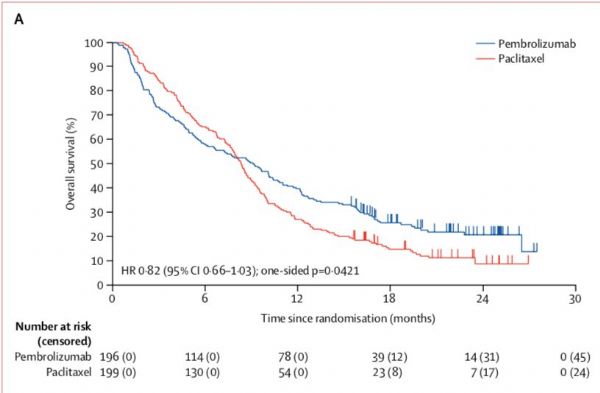
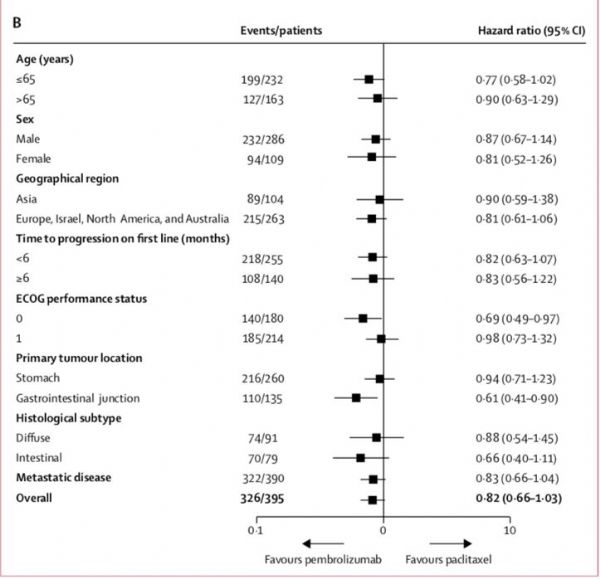
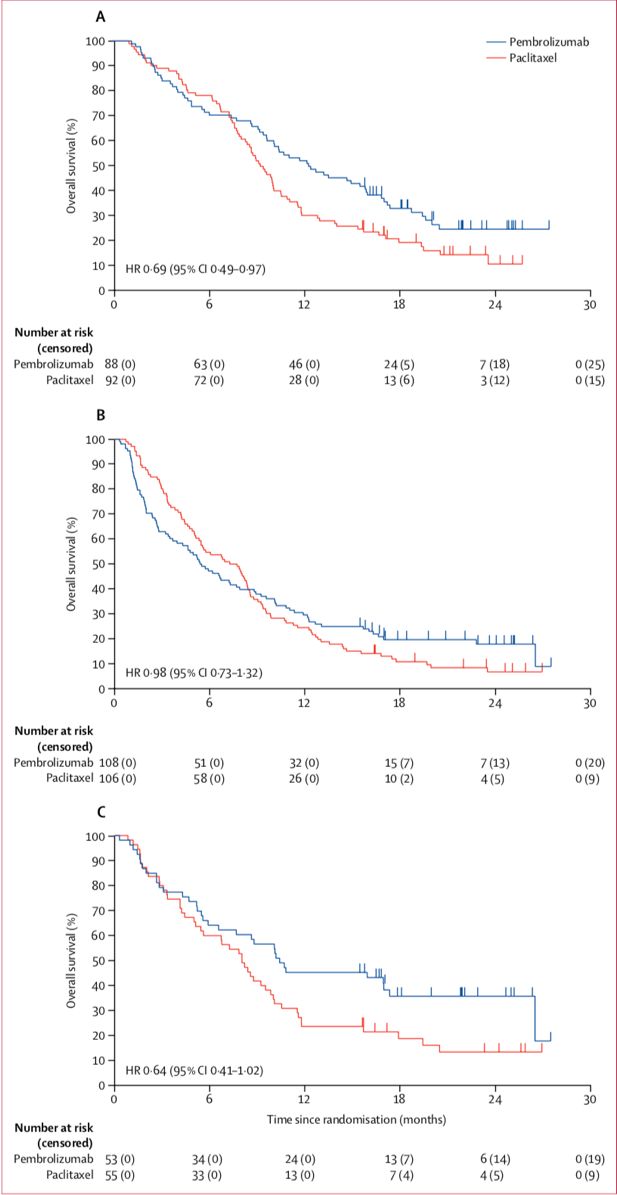
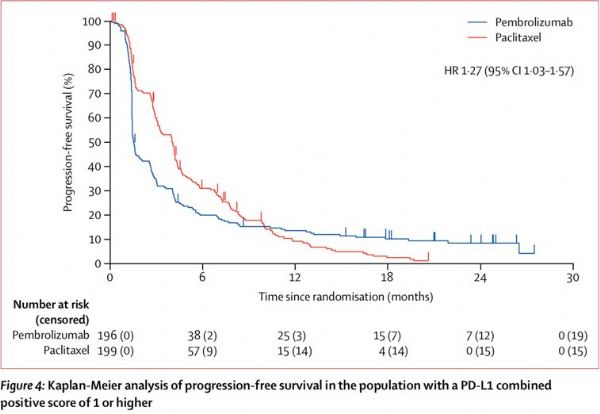
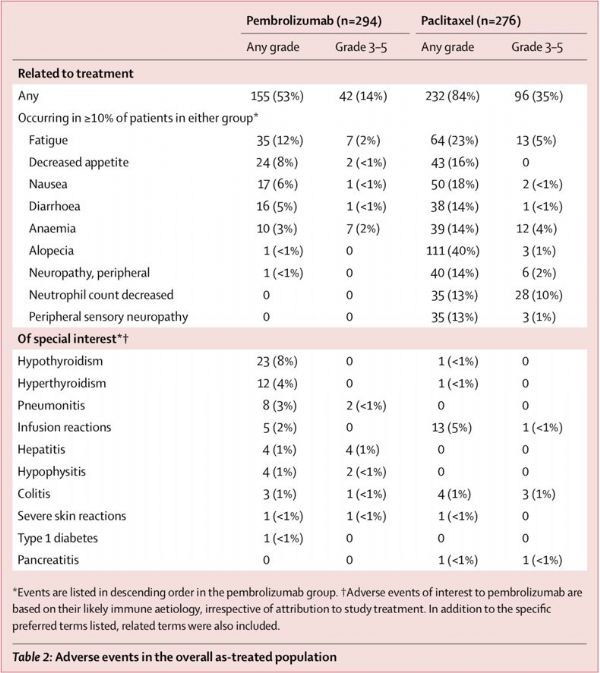
晚期胃癌患者一线治疗后进展者结局通常不佳,而且二线治疗的选择十分有限。但随着免疫检查点阻滞剂的问世,多种肿瘤的治疗模式发生了变化。在晚期胃癌治疗后进展的患者中,免疫检查点阻滞剂是否能同样复制在其他肿瘤中的奇迹呢?KEYNOTE-061研究给了我们答案。遗憾的是,即使是在PD-L1联合阳性评分≥1的复发的晚期胃癌或胃食管结合部癌患者中,帕博利珠单抗二线治疗并未能延长其总生存。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#帕博利珠#
32
#Lancet#
33
微卫星不稳定那部分患者是否比化疗效果更好?
73
#胃食管#
33
#癌症患者#
23
#食管#
23
学习学习再学习
83
阅
72
学习了.谢谢分享
64
一起学习学习
65