Science:对肝脏线粒体功能进行系统蛋白质组学研究
2016-06-10 佚名 生物谷
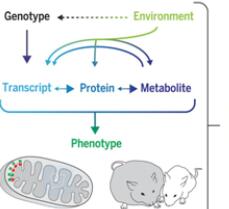
科学家们通过对小鼠开展大规模蛋白质组学研究获得脂肪和能量代谢的分子遗传背景方面的新认识。蛋白质组是一种生物体或某一种细胞、一种组织的基因组所表达的全部蛋白。在一项新的研究中,由瑞士联邦理工学院教授(ETH Zurich)Ruedi Aebersold领导的一个专门从事蛋白质组学研究的团队和由瑞士洛桑联邦理工学院(EPFL)教授Johan Auwerx领导的一个专门从事于线粒体生理学与肝脏疾病研

科学家们通过对小鼠开展大规模蛋白质组学研究获得脂肪和能量代谢的分子遗传背景方面的新认识。蛋白质组是一种生物体或某一种细胞、一种组织的基因组所表达的全部蛋白。在一项新的研究中,由瑞士联邦理工学院教授(ETH Zurich)Ruedi Aebersold领导的一个专门从事蛋白质组学研究的团队和由瑞士洛桑联邦理工学院(EPFL)教授Johan Auwerx领导的一个专门从事于线粒体生理学与肝脏疾病研究的团队合作开展这项突破性的研究项目。就这项研究而言,蛋白质组指的是小鼠肝脏中表达的全部蛋白。相关研究结果发表在2016年6月10日那期Science期刊上,论文标题为“Systems proteomics of liver mitochondria function”。
论文共同第一作者Evan Williams说,“与人类一样,不同小鼠个体之间也存在差异,比如,在胆固醇代谢或脂肪肝等代谢疾病易感性方面存在差异。” Williams作为EPFL的一名博士生开展这项研究,如今是ETH Zurich的是一名博士后研究员。“这些差异中的一些能够从遗传学的角度加以解释,但是并不是所有的差异都是如此”,他说。
最新的技术
研究人员将来自一个大型小鼠群体的综合性蛋白数据汇集在一起,从而有助他们解释额外的代谢差异。他们采用一种被称作SWATH-MS的质谱测量技术,这种技术是由ETH Zurich的Aebersold团队最近开发出来的。它允许研究人员测量这种实验性小鼠肝脏中一系列蛋白的浓度。
论文共同第一作者、Aebersold团队博士生研究员Yibo Wu解释道,“测量蛋白质组要比对整个基因组进行测序更加复杂得多。利用SWATH-MS技术,测量上百个样品中的上千种不同的蛋白是可行的。”在这项研究中,研究人员测量了小鼠肝脏组织样品中的2600种不同的蛋白。为了开展这些蛋白质组测量,一种庞大的蛋白数据库是必需的;Wu在近几年构建这种小鼠蛋白数据库中发挥着主导作用。
蛋白质组作为基因组的补充
研究人员研究的一群小鼠是由40种小鼠品系组成的,这些小鼠品系可追溯到两个相同的祖先,因此彼此之间的亲缘关系比较密切。由来自这些10种小鼠品系的代表性小鼠组成多组相同的小鼠,给它们喂食高脂肪食物(即人们所述的垃圾食品)或健康的低脂肪食物。在几周之后,他们记录了这些小鼠的常规医学(生理学)数据,尤其是测试了它们的表现和它们如何快地通过身体活动降低它们的体重。正如研究人员期待中的那样,这些小鼠对高脂肪食物摄入作出不同的反应。一些小鼠患上代谢疾病,如脂肪肝,但是其他小鼠则不会如此。
为了进行评估,研究人员将这些生理学数据与基因组、转录组和蛋白质组数据结合在一起。从这些结合的数据中,他们能够更加准确地描述几种特定的蛋白在脂肪和能量代谢中的作用。其中一种蛋白是COX7A2L。他们发现,在小鼠体内,这种蛋白负责形成在线粒体---细胞内部的能量工厂---中发现的超级蛋白复合体(supercomplex)。这种超级蛋白复合体由100多种不同的蛋白组成,负责以合适的形式给细胞提供所需的能量。具有太少COX7A2L蛋白的小鼠不能够提供足够数量的所需能量,因而给整个有机体带来负面影响。
在个人化医疗中的应用
这项研究是迄今为止利用SWATH-MS技术在哺乳动物体内开展的最为完整的蛋白质组学研究。由ETH Zurich科学家们开发的这种技术也准备在人体中开展群体研究:Aebersold团队已为上千种人蛋白构建出一个对应的数据库。Aebersold说,“正如这项研究中的小鼠品系一样,每个病人在遗传上存在差异。我们在小鼠群体中使用的这种方法如今能够以一种疾病接着一种疾病的方式用于人类疾病研究,特别是对个人化医疗而言。”
原始出处
Evan G. Williams1,*, Yibo Wu2,*, Pooja Jha1, Sébastien Dubuis2, Peter Blattmann2, Carmen A. Argmann3, Sander M. Houten3, Tiffany Amariuta1, Witold Wolski2, Nicola Zamboni2, Ruedi Aebersold2,4,†, Johan Auwerx.Systems proteomics of liver mitochondria function.Science.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#白质#
23
#线粒体功能#
32
#蛋白质组#
32
#组学研究#
44
#蛋白质#
37
#SCIE#
27
未来临床的需要
103
这图漂亮
60
的确高深
155
好好学习
100