Cell Death & Disease:miR-361-3p能够增加前列腺癌对恩杂鲁胺的敏感性
2020-10-12 AlexYang MedSci原创
缺少配体结合域的雄激素受体剪接变异体7(ARv7)越来越被认为是导致前列腺癌(PCa)患者对恩杂鲁胺(Enz)耐药的关键因子。然而,ARv7的表达是如何被调控的详细机制以及它是否需要其他因子来诱导最大
缺少配体结合域的雄激素受体剪接变异体7(ARv7)越来越被认为是导致前列腺癌(PCa)患者对恩杂鲁胺(Enz)耐药的关键因子。然而,ARv7的表达是如何被调控的详细机制以及它是否需要其他因子来诱导最大的Enz耐药性仍不清楚。
最近,有研究人员鉴定了miR-361-3p在复发性PCa患者中的表达较低,能够通过结合到ARv7的3′UTR发挥功能(但不与野生型AR结合),抑制其表达从而增加Enz敏感性。重要的是,研究人员发现miR-361-3p也可以与MAP激酶相互作用的丝氨酸/苏氨酸激酶2(MKNK2)的3′UTR结合,并抑制其表达以进一步增加Enz敏感性。反过来,Enz的增加可以通过改变HIF-2α/VEGFA信号的反馈机制,在缺氧条件下抑制miR-361-3p的表达。利用原位异种移植CWR22Rv1细胞的体内小鼠模型进行的临床前研究表明,将Enz与小分子miR-361-3p结合使用能够更好地抑制Enz耐药性PCa肿瘤的进展。
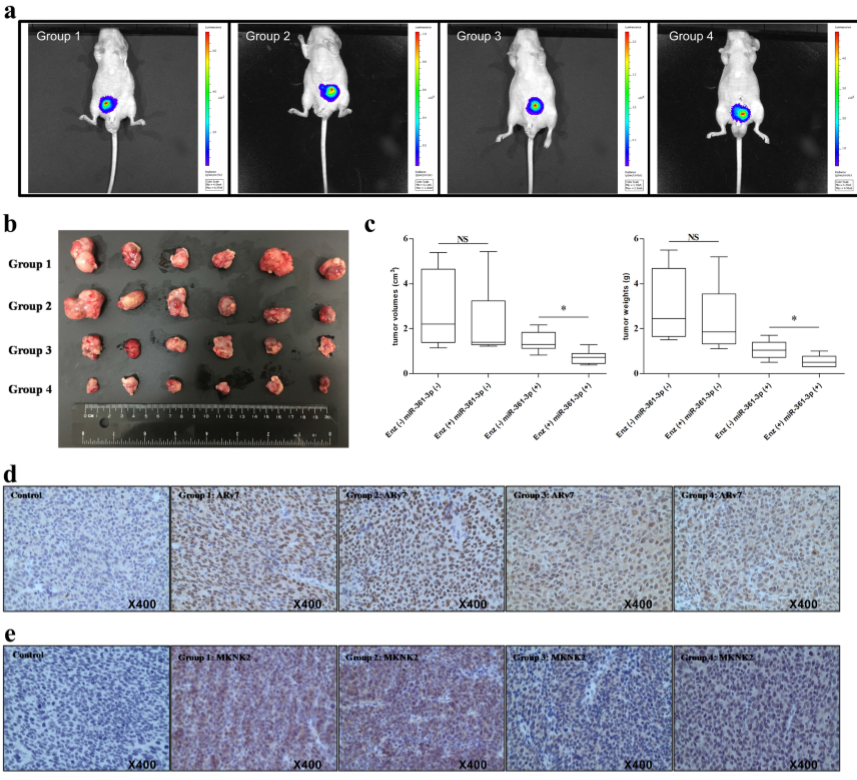
体内试验表明miR-361-3p能够抑制Enz抗性前列腺癌(PCa)肿瘤
总的来讲,这些预临床研究共同阐释了miR-361-3p可以通过抑制ARv7和MKNK2的表达来最大限度地提高Enz的敏感性,用小分子靶向这些新发现的Enz/miR-361-3p/ARv7和/或Enz/miR-361-3p/MKNK2信号可能有助于开发新的疗法,从而更好地抑制已经发展为Enz耐药患者的CRPC。
原始出处:
Bianjiang Liu, Yin Sun, Min Tang et al. The miR-361-3p increases enzalutamide (Enz) sensitivity via targeting the ARv7 and MKNK2 to better suppress the Enz-resistant prostate cancer. Cell Death & Disease. Sep 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
36
#CEL#
27
#miR#
33
#Dis#
26
#敏感性#
41
#Death#
37
前列腺癌相关研究,学习了,谢谢梅斯
50