European Radiology:看骨髓水肿,双能CT也能做到!急性椎体骨折的附加诊断
2022-01-20 shaosai MedSci原创
在脊柱创伤的情况下,根据骨折线的特定形态学标志对急性椎体骨折进行影像学诊断具有挑战性,尤其是对于出现老年骨质疏松性骨折的老年患者来说难度更大。
 在脊柱创伤的情况下,根据骨折线的特定形态学标志对急性椎体骨折进行影像学诊断具有挑战性,尤其是对于出现老年骨质疏松性骨折的老年患者来说难度更大。在这种情况下,检测骨髓水肿(BME)作为急性损伤的标志可以大大促进更准确的诊断。
在脊柱创伤的情况下,根据骨折线的特定形态学标志对急性椎体骨折进行影像学诊断具有挑战性,尤其是对于出现老年骨质疏松性骨折的老年患者来说难度更大。在这种情况下,检测骨髓水肿(BME)作为急性损伤的标志可以大大促进更准确的诊断。
磁共振成像(MRI)可以充分显示BME,是目前诊断急性椎体骨折的成像金标准。然而,磁共振成像在骨骼显示及扫描方面具有局限性。
计算机断层扫描(CT)由于空间分辨率高,检查时间短,是骨质结构和骨折线形态学评估的金标准。然而,传统CT对BME的显示由于覆盖在骨髓上的小梁骨而受到影响[8]能力有限。随着CT技术的发展,双能量CT(DECT)通过应用两种不同的X射线能量谱,能够克服这一局限性。DECT衍生的虚拟非钙质(VNCa)图像可以减去骨小梁上的钙质信号,实现BME的可视化。然而到目前为止,还没有研究对DECT和MRI的两种信息进行综合分析,这对于准确评估脊柱创伤的严重程度和及时启动相应的治疗可能具有特殊的临床意义。
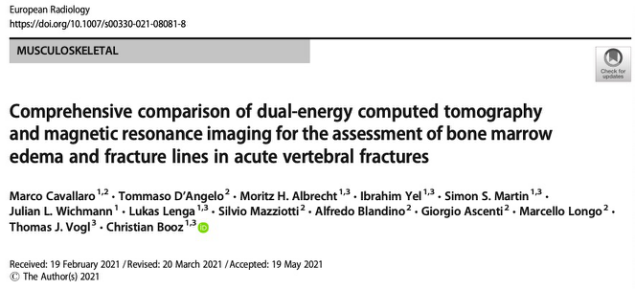
近日,发表在European Radiology杂志的一项研究比较了DECT和MRI在急性椎体骨折的情况下,两者的诊断准确性、诊断置信度、评估骨折线和BME的图像质量方面之间的差异,为椎体骨折患者的早期准确诊断及治疗提供了技术支持。
对接受双源DECT和3T脊柱MRI检查的88名连续患者进行了回顾性分析。五位放射科医生评估了所有椎体BME的存在和程度,以及MRI和12周后DECT图像中急性骨折线的识别。此外,还评估了图像质量、图像噪声比以及对急性椎体骨折的整体诊断信心。CT数字的定量分析是由第六位放射科医生进行的。两位放射科医生分析了MRI和灰阶DECT图像,以确定参考标准。
对于评估BME的存在和程度,DECT显示出高灵敏度(分别为89%和84%)和特异性(两者均为98%),与MRI相比,DECT检测BME的诊断置信度也同样高(2.30 vs. 2.32;范围0-3)(P = .72)。对于评估急性骨折线,MRI达到了较高的特异性(95%),中等的敏感性(76%),与DECT相比,诊断置信度明显较低(2.42 vs. 2.62,范围0-3)(p < .001)。诊断BME的截止值为-0.43HU,其敏感性为89%,特异性为90%,总体AUC为0.96。
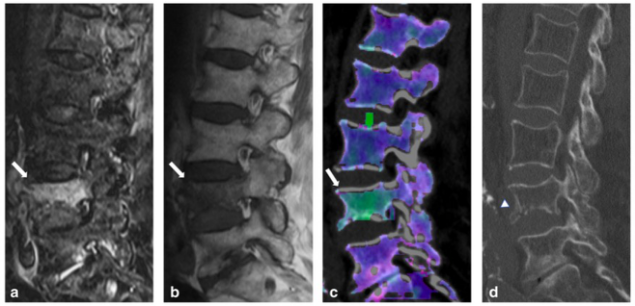
图 87 岁,女性因跌倒而出现急性脊柱外伤。a TIRM–MRI序列,b SE T1 加权MRI序列,c DECT–VNCa重建图像显示L4的所有四个象限(箭头)的骨髓水肿(BME)。所有读者在评估两种技术的 BME 存在(3 分 = 不同的 BME)和范围(4 分 = 所有象限)方面是一致的。d DECT图像检测 L1(箭头)的急性轻微骨折,该骨折为与不稳定性相关的泪滴状骨折。 在MR和DECT图像中,所有的读者将描绘骨折线的信心分别评为中等(2 分)和高(3 分)。
本研究表明,DECT和MRI对急性椎体骨折的评估都有很高的诊断可信度和图像质量。DECT通过VNCa重建,为评估椎体BME的存在和程度提供了高诊断准确性。MRI对骨折线的描述显示出中等的敏感性和较低的可信度。因此,在急性脊柱创伤的特定情况下,DECT是无法行MRI检查患者的替代成像方法,特别是在老年人或不稳定的病人以及细微或复杂方向的骨折线的情况下。
原文出处:
Marco Cavallaro,Tommaso D'Angelo,Moritz H Albrecht,et al.Comprehensive comparison of dual-energy computed tomography and magnetic resonance imaging for the assessment of bone marrow edema and fracture lines in acute vertebral fractures.DOI:10.1007/s00330-021-08081-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#椎体骨折#
49
#PE#
26
#双能CT#
50
#水肿#
42
#椎体#
62