JCEM:质子泵抑制剂对血糖控制和糖尿病事件的影响
2021-07-05 MedSci原创 MedSci原创
接受PPI治疗改善了糖尿病患者的血糖指数,但并未改变糖尿病发生风险。因此,在给糖尿病患者开抗酸药时,应考虑PPI对血糖控制的影响。
质子泵抑制剂(PPI)是否可以改善糖尿病患者的血糖控制或降低普通人群发生糖尿病的风险尚未明确。

近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员旨在评估PPI治疗对糖尿病患者血糖控制以及对糖尿病发生风险的影响。
 研究人员检索了PubMed、Embase、Scopus和ClinicalTrials.gov等数据库,检索时间从数据库成立到2020年11月21日。研究人员纳入了比较接受和未接受PPI治疗的糖尿病患者糖化血红蛋白(HbA1c)或空腹血糖(FBG)的研究。这些研究评估了服用PPI治疗的患者发生糖尿病的风险。研究人员进行了双重独立审查、数据提取和质量评估,并使用随机效应模型估算了组间的加权平均差异或相对风险。
研究人员检索了PubMed、Embase、Scopus和ClinicalTrials.gov等数据库,检索时间从数据库成立到2020年11月21日。研究人员纳入了比较接受和未接受PPI治疗的糖尿病患者糖化血红蛋白(HbA1c)或空腹血糖(FBG)的研究。这些研究评估了服用PPI治疗的患者发生糖尿病的风险。研究人员进行了双重独立审查、数据提取和质量评估,并使用随机效应模型估算了组间的加权平均差异或相对风险。
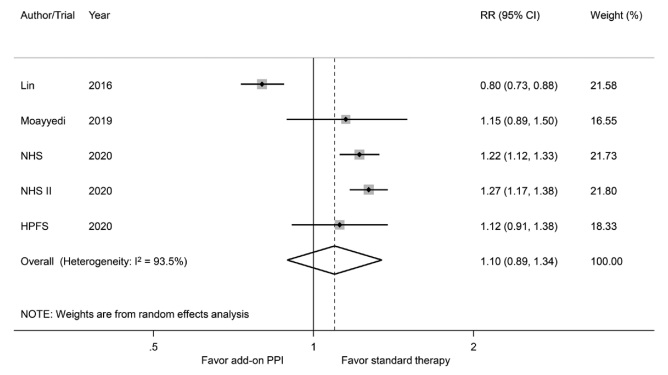 PPI治疗与糖尿病发生的相对风险
PPI治疗与糖尿病发生的相对风险
该系统评价纳入了七项血糖控制研究(n=342)和5项评估糖尿病发生风险的研究(n=244439)。与标准治疗相比,接受PPI治疗与HbA1c(WMD为-0.36%;95%CI为-0.68至-0.05;P=0.025)和FBG(WMD为-10.0mg/dL;95%CI为-19.4至-0.6;P=0.037)显著降低相关。接受PPI治疗并未降低糖尿病发生风险(合并RR为1.10;95%CI为0.89至1.34;P=0.385)。
由此可见,接受PPI治疗改善了糖尿病患者的血糖指数,但并未改变糖尿病发生风险。因此,在给糖尿病患者开抗酸药时,应考虑PPI对血糖控制的影响。
原始出处:
Carol Chiung-Hui Peng.et al.Effects of Proton Pump Inhibitors on Glycemic Control and Incident Diabetes: A Systematic Review and Meta-Analysis.JCEM.2021.https://doi.org/10.1210/clinem/dgab353
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JCEM#
35
#抑制剂#
35
#JCE#
37
#质子泵#
45
学习了
67
#血糖控制#
39
谢谢MedSci提供最新的资讯
61
学习了
64