Br J Cancer:质子泵抑制剂PPI的使用影响结直肠癌患者的生存率
2021-07-13 xiaozeng MedSci原创
质子泵抑制剂(PPI)是全球最常用的处方药之一,在所有成年人中的使用率高达11-30%。
质子泵抑制剂(PPI)是全球最常用的处方药之一,在所有成年人中的使用率高达11-30%。然而,由于其潜在的致癌作用和其他主要的健康并发症,长期使用PPI的安全性越来越受到质疑。
既往研究显示,PPI可以改变肠道微生物群的丰富度和多样性。根据临床前研究的证据,其引起的肠道生态失调可能导致结直肠癌(CRC)的发生发展。因此,该研究旨在评估PPI的使用与CRC特异性死亡率之间的相关性。
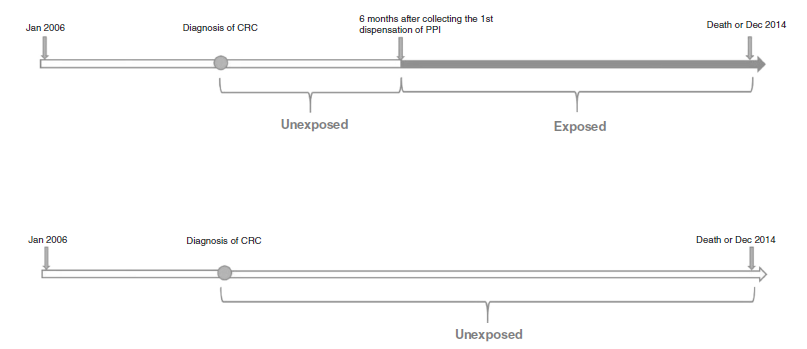
研究人员收集了2006年至2012年期间在瑞典处方药登记处注册的所有被诊断患有CRC的患者(N=32,411,54.9%PPI使用者),随后通过瑞典死因登记处的登记链接跟踪患者直到2013年12月。
结果显示,共有4746名(14.0%)患者死亡,PPI使用者和PPI非使用者的全因死亡率的aHR(调整后风险比)为1.38。在男性、癌症0-I期、直肠癌和接受CRC手术的患者中观察到更高的关联型。
使用PPI的全因死亡率相关性在新使用者与非使用者之间的比较(aHR=1.47)相比于在连续使用者与非使用者之间(aHR=1.32)更为显著。PPI使用者与PPI非使用者的CRC特异性死亡率的风险估计值与患者的全因死亡率的风险估计值相似。
PPI的使用与CRC的诊断相关
总而言之,该研究结果揭示,在诊断CRC后使用PPI与患者的全因死亡率和CRC特异性死亡率的增加相关。
原始出处:
Wang, X., Liu, Q., Halfdanarson, ó.Ö. et al. Proton pump inhibitors and survival in patients with colorectal cancer: a Swedish population-based cohort study. Br J Cancer (12 July 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
34
#质子泵#
48
学习了
92
#生存率#
40
#结直肠#
35