Circulation:PCSK9抑制剂阿利库单抗对急性冠脉综合征患者卒中风险的影响
2019-12-22 QQY MedSci原创
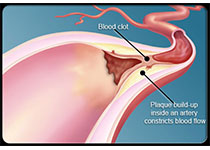
降低致动脉粥样硬化脂蛋白,包括低密度脂蛋白胆固醇(LDL-C),可降低缺血性卒中的风险。但低LDL-C水平和出血性卒中的潜在风险增加引起了人们的关注。ODYSSEY OUTCOMES试验在18 924位急性冠脉综合征合并粥样硬化脂蛋白升高的患者中对比了PCSK9抑制剂阿利库单抗和安慰剂的效果。这项预先指定的分析旨在评估阿利库单抗对缺血性和出血性卒中的影响。患者在急性冠脉综合征后1-12个月被随机分
患者在急性冠脉综合征后1-12个月被随机分至阿利库单抗组或安慰剂组。评估非致死性或致死性缺血性或出血性卒中的风险,并根据基线LDL-C浓度和脑血管病史进行分层。还评估了在第4个月时阿利库单抗治疗获得极低的LDL-C水平与以及随后的出血性卒中之间的潜在联系。
中位随访2.8年。共发生263例缺血性和33例出血性卒中。在不增加出血性卒中风险(HR, 0.83 [95% CI, 0.42?1.65])的情况下,阿利库单抗治疗可降低任何卒中(HR 0.72[95% CI 0.57-0.91])和缺血性卒中(HR, 0.73 [95% CI, 0.57?0.93])的风险。总体上,起始LDL-C<80、80~100和>100mg/dL的患者分别有7164人(37.9%)、6128人(32.4%)和5629人(29.7%)。起始LDL-C较高的患者对卒中的治疗效果更显著,但无正式的异质性证据。有无脑血管病史不影响使用阿利库单抗对卒中的影响。在阿利库单抗组中,低LDL-C与出血性卒中发生率之间无明显的不良关系。
对于采用强化他汀类药物治疗的新确诊的急性冠脉综合征和血脂异常的患者,使用阿利库单抗治疗可降低患者的卒中风险。此外,出血性卒中的风险与阿利库单抗组所获得的LDL-C水平无关。
原始出处:
J. Wouter Jukema, et al.Effect of Alirocumab on Stroke in ODYSSEY OUTCOMES.Circulation. 2019;140:2054–2062
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
32
#阿利库单抗#
47
#PCSK9抑制#
54
#Csk#
35
#PCS#
33
#卒中风险#
24
#综合征#
33
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
52
中风是俗称,应该称为缺血性卒中吧
46