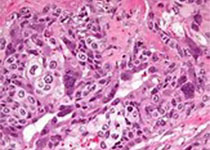
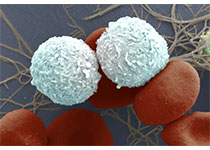
Oncogene:靶向加压素2型受体治疗肾细胞癌研究
2019-10-25 AlexYang MedSci原创
精氨酸后叶加压素(AVP)和其2型受体(V2R)在肾脏的盐分和水分稳态调控中具有必要的作用。体外试验中,V2R激活能够刺激肾细胞肿瘤(RCC)细胞系的增殖。最近,有研究人员在人类RCC肿瘤中调查了V2R表达和活性,以及其在RCC肿瘤生长中的作用。研究人员通过对癌症基因组数据库(TCGA)的调查,人类RCC肿瘤组织芯片的分析以及cDNA和肿瘤组织样本分析阐释了V2R表达和在透明细胞RCC(ccRCC
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
39
#加压素#
38
#Gene#
33
#Oncogene#
35