探索头条:重磅发现!Nature子刊连发两文:癌细胞“休眠”数年不死 或是导致癌症转移/复发的关键因素
2021-12-21 生物探索 网络
在我国,白血病的发病率在各类肿瘤中占据第六位,而患病人群中又以低龄儿童为多。

End
参考资料:
[3]https://baijiahao.baidu.com/s?id=1718716616366065347&wfr=spider&for=pc
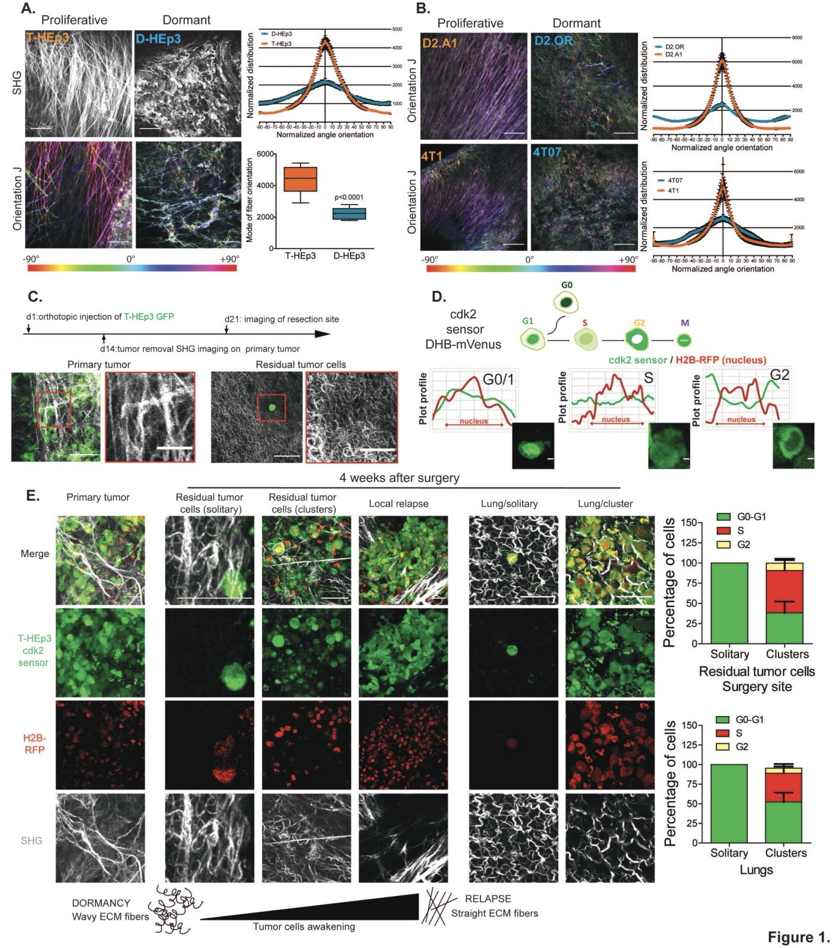
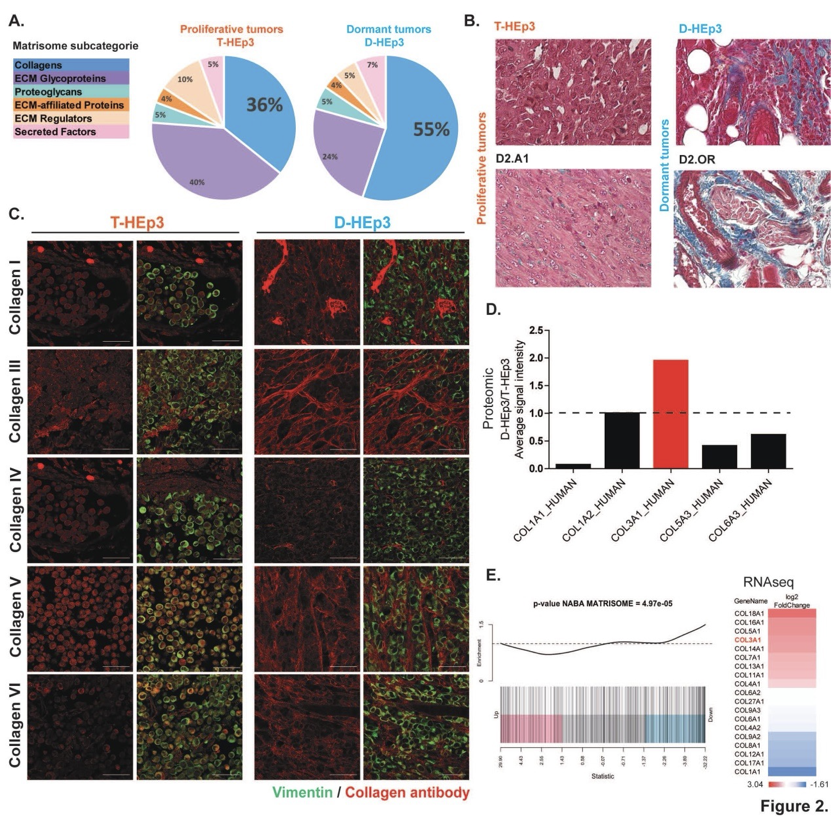
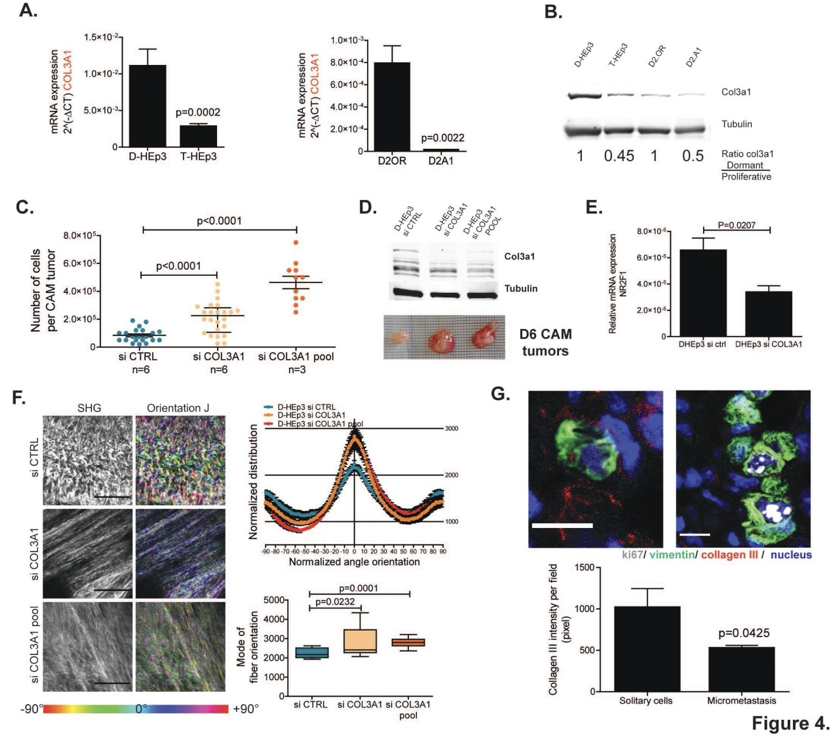
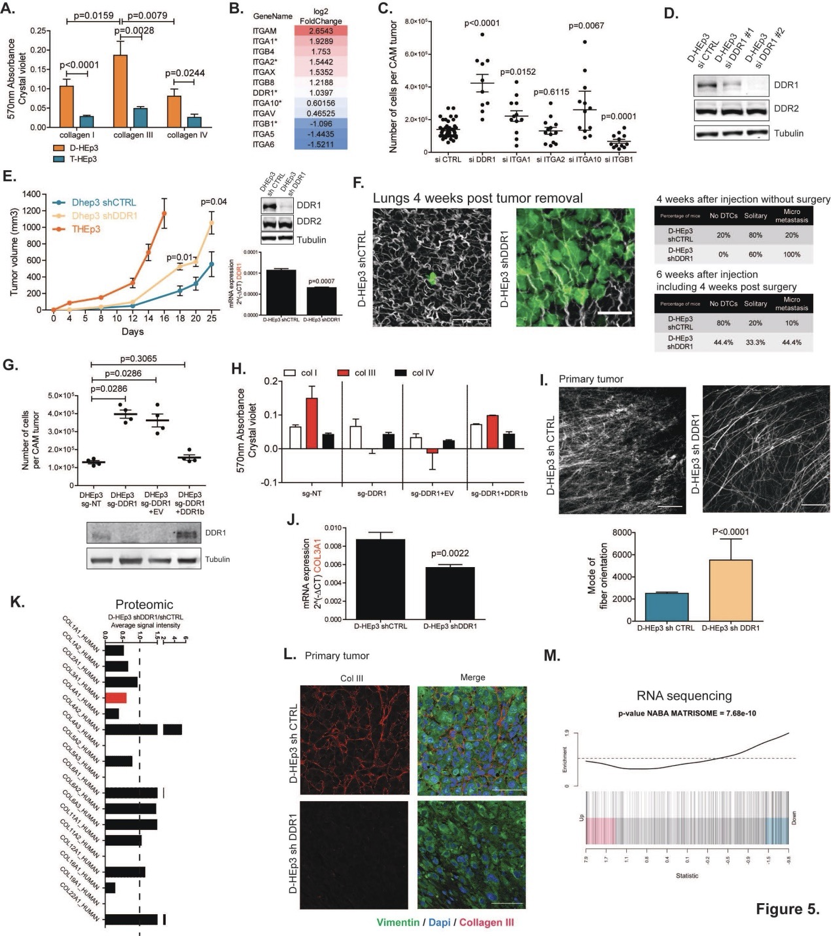
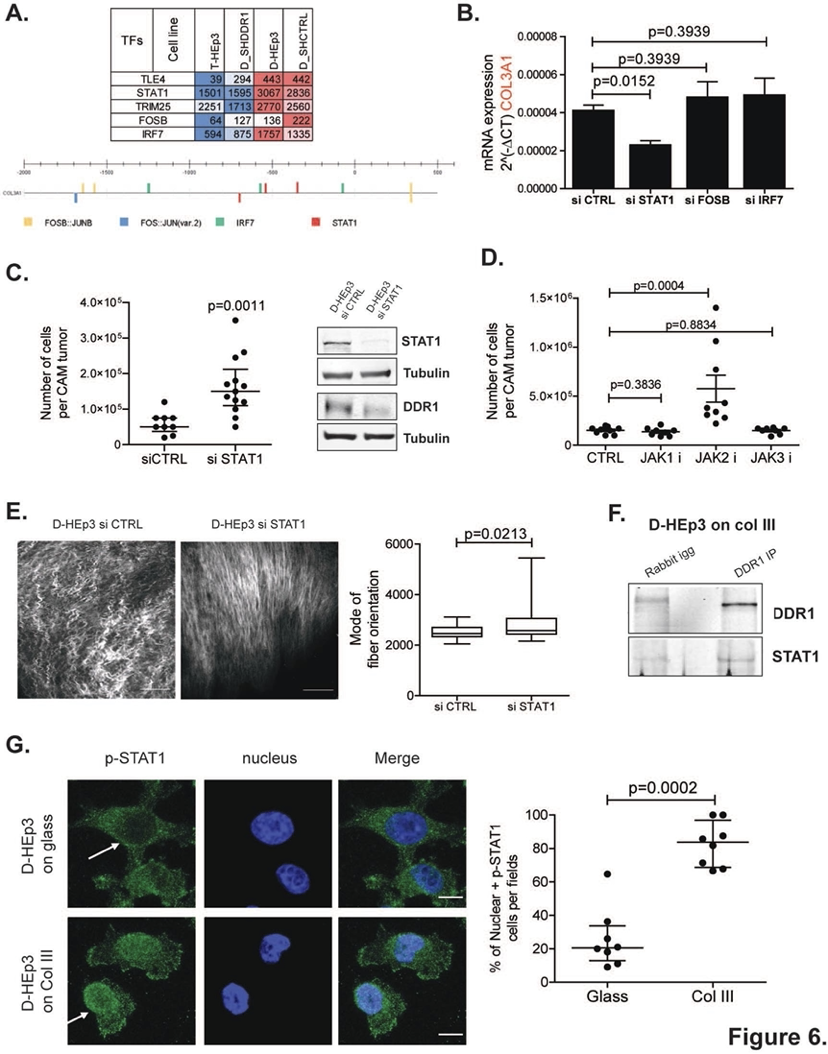
[4]Martino JD, Nobre AR, Mondal C, et al. A tumor-derived type III collagen-rich ECM niche regulates tumor cell dormancy [J]. Nature Cancer 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#休眠#
41
#Nat#
29
#癌细胞#
0
#致癌#
29
#癌症转移#
40
#重磅#
26
学习
0