NEJM重磅证据:大面积急性脑梗也应该及时进行血管内治疗!
2022-05-02 MedSci原创 MedSci原创
大面积脑梗死患者接受血管内治疗比单独接受内科治疗有更好的功能结局,但颅内出血风险增加。
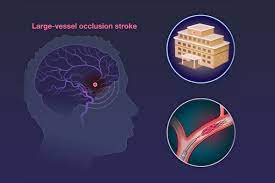
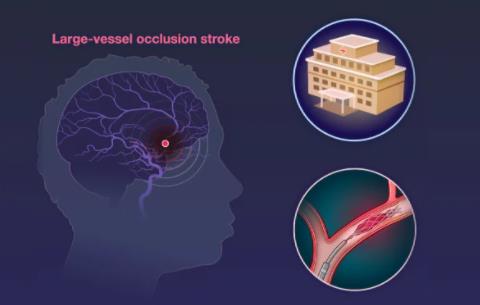
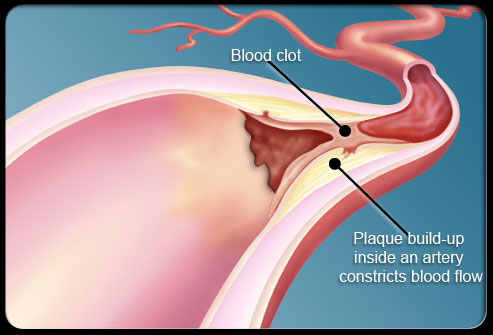
血管内治疗已成为大血管闭塞急性缺血性卒中的标准治疗方法之一。急性缺血性卒中的血管内治疗一般在大面积梗死的患者(例如,ASPECTS值为≤5)避免使用,但血管内治疗配合医疗护理与单纯医疗护理对大面积卒中的效果还没有很好的研究。
为此,来自日本的学者进行了一项名为RESCUE-Japan LIMIT多中心、开放标签、随机的临床试验,涉及大脑血管闭塞和影像学上的大面积脑卒中患者,即ASPECTS值(0-10,值越低表示梗死越大)为3-5的患者,结果发表在NEJM杂志上。

患者按1:1的比例随机分配,在他们最后一次被告知情况良好后的6小时内接受血管内治疗和医疗护理,或在24小时内(如果流体衰减反转恢复图像上没有早期变化)接受医疗护理。两组都在适当的时候使用rtPA。主要结果是90天后mRS评分为0-3分。次要结果包括在90天内mRS得分向更好的结果转变,以及在48小时内 NIHSS得分提高≥8分。
结果共有203名患者接受了随机化治疗;101名患者被分配到血管内治疗组,102名患者被分配到医疗护理组。每组中约有27%的患者接受rtPA。90天后,血管内治疗组中mRS评分为0-3分的患者比例为31.0%,医疗护理组为12.7%(RR=2.43;95%CI,1.35-4.37;P=0.002),提示mRS评分范围内的顺序变化有利于血管内治疗。

在48小时内,有31.0%的血管内治疗组患者和8.8%的医疗护理组患者的NIHSS评分改善了至少8分(RR=3.51;95%CI,1.76-7.00),并且分别有58.0%和31.4%的患者发生颅内出血。
综上,在日本进行的一项试验中,大面积脑梗死患者接受血管内治疗比单独接受内科治疗有更好的功能结局,但颅内出血风险增加。
参考文献:
Endovascular Therapy for Acute Stroke with a Large Ischemic Region. N Engl J Med. 2022 Apr 7;386(14):1303-1313. doi: 10.1056/NEJMoa2118191.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#大面积#
32
#脑梗#
47
#重磅#
40
很前沿的咨询,谢谢分享!!!
54
NEJM上果然牛,感谢梅斯更新及时
28
#缺血性卒中#的#血管内治疗#
114