肥胖与高血压,关系大了|AHA科学声明
2021-10-17 中国医学论坛报今日循环 中国医学论坛报今日循环
高血压的危害性相信不用再强调,大家耳熟能详。如何预防高血压,也是无数相关工作者一直在探索的方向。
高血压的危害性相信不用再强调,大家耳熟能详。如何预防高血压,也是无数相关工作者一直在探索的方向。
与其他因素相比,有个与高血压息息相关的重要因素却被远远低估了!
那就是:肥胖!
导致高血压的各类因素研究显示,肥胖能够通过神经激素激活、炎症和肾功能障碍等多种机制导致原发性高血压。
而肉眼可见的事实是,现代社会肥胖患病率不断增加,高血压相关的心血管及肾脏疾病风险也随之增加。
如何有效减肥,成了维持健康的重要问题。
近日,美国心脏协会(AHA)最新共识——预防和治疗高血压的减重策略,在线发表于《高血压》(Hypertension)杂志。
新版共识为高血压合并肥胖患者的减重指出了方向。为了预防、治疗高血压,减重是必须要做的事!
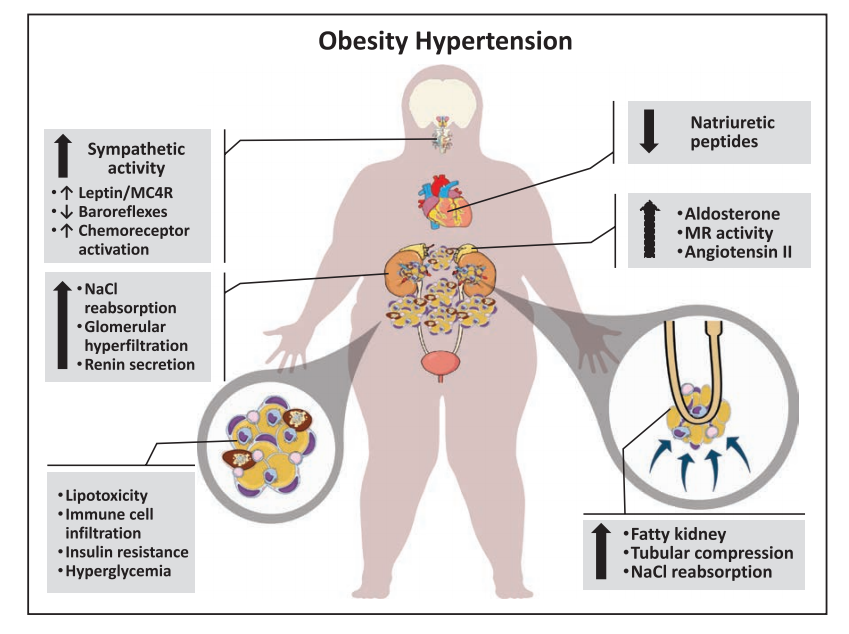
▲肥胖对血压升高的影响是多因素的,涉及神经激素的改变、脂肪对肾脏的物理压迫、氯化钠重吸收的增加,以及炎症反应等。
通常肥胖患者会以改善生活方式的办法来达到减肥的目的,如:改变饮食习惯,减少久坐,增加体力活动等。
减少久坐?对上班族来说好像有点困难。
加强锻炼?似乎对大多数人来说,规律运动并且长久坚持下来,确实不是一件容易的事。
如此看来,优化饮食习惯好像是更为简单易行、可长期坚持的方法。
那饮食习惯对减肥和高血压控制的影响到底怎么样的呢?真的会有效果吗?
目前的饮食指南强调基于饮食模式的方法预防和控制疾病,当前比较推荐的健康饮食模式包括地中海饮食和DASH饮食等。
这两种饮食模式都含有:
丰富的水果、蔬菜、豆类、坚果和种子;
适量的鱼类、海鲜、家禽和乳制品;
少量的红肉和加工肉类和糖果。
此外,地中海饮食还建议使用橄榄油和定期但适度地食用葡萄酒(尤其是红酒)。
改善饮食的效果怎么样呢?
1、地中海饮食
2019年科克伦(Cochrane)对随机对照试验回顾发现,地中海饮食可降低收缩压3.0 mmHg(95%CI:2.5~3.5 mmHg),降低舒张压2.0 mmHg(95%CI:1.7~2.3 mmHg)。
另外一项纳入16项随机对照试验的荟萃分析发现,地中海饮食可以降低体重1.8kg(95%CI:0.6~2.9 kg),降低BMI 0.6 kg/m²(95%CI:0.2~0.9 kg/m²)。
2、DASH饮食
在纳入24项饮食模式干预随机对照试验的荟萃分析中发现,DASH饮食可降低收缩压7.6 mmHg(95%CI:5.3~10.0 mmHg),降低舒张压4.2 mmHg(95%CI:2.6~5.9 mmHg)。
当DASH饮食与运动及低钠饮食结合时,降压效果更明显。
3、低钠饮食
对133项随机对照试验的分析显示,在血压> 131/78 mmHg的人群中,钠摄入量减少2.3 克/天,收缩压可降低7.7 mmHg(95%CI:5.0~10.4 mmHg),舒张压可降低3.0 mmHg(95%CI:1.4~4.6 mmHg)。
4、间歇性禁食
对4项随机对照试验的系统回顾显示,虽然间歇性禁食对短期减肥有效,但其对血压降低的影响较弱。
中国营养学会组织编写的《中国居民膳食指南科学研究报告(2021)》中也提到了相关内容。
2017年中国居民310万人的死亡可归因于膳食不合理,其中高血压和糖尿病比较明显。
而高钠摄入在成人膳食因素导致心血管代谢性疾病死亡中占第一位(17.3%),第二位和第三位分别是水果摄入不足(11.5%)和水产类Ω-3脂肪酸摄入不足(9.7%)。
能够降低主要健康结局风险的膳食因素包括:全谷物、蔬菜、水果、大豆及其制品、奶类及其制品、鱼肉、坚果、饮水(饮茶)等。
过多摄入可增加不良健康结局风险的膳食因素有:畜肉、烟熏肉、食盐、饮酒、含糖饮料、油脂等。
这是不是与DASH饮食及地中海饮食不谋而合?
其实,今年在AHA关于1型糖尿病的声明中就强调了地中海饮食的重要性。
如何快速判断饮食是否合理?
下面是几份简单的问卷,可以在实际应用中参考。
“地中海饮食筛查”
(Mediterranean Diet Adherence Screener,MEDAS)
1.你是否用橄榄油作为烹饪的主要脂肪来源?
2.你每天用多少橄榄油(包括油炸,外食,沙拉等)?
3.你每天吃多少份蔬菜?
4. 你每天吃多少水果(包括鲜榨果汁)?
5. 你每天吃多少红肉、汉堡包或肉制品(火腿、香肠等)?
6. 你每天吃多少份黄油、人造黄油或奶油?
7. 你每天喝多少含糖饮料?
8. 你每周喝多少酒?
9. 你每周吃多少次豆类制品?
10. 你每周吃多少鱼或贝类/海鲜?
11. 你每周吃多少次糖果或糕点(不是自制的),如蛋糕、饼干、饼干等?
12. 你每周吃多少坚果?
13. 你更喜欢吃鸡肉、火鸡肉或兔肉而不是牛肉、猪肉、汉堡包或香肠吗?
14. 你每周吃几次用橄榄油煸炒的番茄、大蒜、洋葱或韭菜制成的蔬菜、意大利面、米饭或其他菜肴?
“快速进食评估”
(Rapid Eating Assessment for Participants,REAP-S)
平均每周,你多久会:
1. 不吃早餐?
2. 外食(包括外卖)≥4顿饭?
3. 每天吃低于2份的全麦食品或高纤维淀粉?
4. 每天吃少于2份水果?
5. 每天吃少于2份的蔬菜?
6. 每天吃或喝少于2份的牛奶、酸奶或奶酪?
7. 每天吃8盎司的肉,鸡肉,火鸡肉或鱼?
8. 吃普通的加工肉类(腊肠、意大利腊肠、咸牛肉、热狗、香肠或培根)而不是低脂加工肉类(烤牛肉、火鸡肉、瘦火腿)?
9. 吃油炸食品,如炸鸡、炸鱼、炸薯条、炸大蕉、土豆泥等?
10. 吃普通的薯片、烤土豆片、玉米片、饼干或普通的爆米花,而不是无盐坚果或空气爆爆米花?
11. 在餐桌上向面包、土豆、米饭或蔬菜中添加黄油或人造黄油?
12. 吃糖果,如蛋糕,饼干,糕点,甜甜圈,松饼,巧克力,和糖果>2次/天?
13. 喝≥16盎司的非减肥苏打水/水果饮料?
14. 通常是购买食材和在家烹饪,而不是外食或点外卖?
15. 去购买食材或做饭是否让你感觉良好?
“鲍威尔和格林伯格测评”
(Powell and Greenberg Screening Tool)
1. 你每周有几次吃蔬菜水果≥5份?
2. 你多久吃一次含糖的食物/饮料(果汁、咖啡或茶中的甜味剂、含糖苏打水)?
参考文献
1. Hall ME, Cohen JB, Ard JD, Egan BM, Hall JE, Lavie CJ, Ma J, Ndumele CE, Schauer PR, Shimbo D; American Heart Association Council on Hypertension; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Lifestyle and Cardiometabolic Health; and Stroke Council. Weight-Loss Strategies for Prevention and Treatment of Hypertension: A Scientific Statement From the American Heart Association. Hypertension. 2021 Sep 20:HYP0000000000000202.doi:10.1161/HYP.0000000000000202. Epub ahead of print. PMID: 34538096.
2. 王崇民. 《中国居民膳食指南科学研究报告(2021)》正式发布[J]. 食品安全导刊,2021(7):15.
3. Daniel W. Jones, et al., (2021). Management of Stage 1 Hypertension in Adults With a Low 10-Year Risk for Cardiovascular Disease: Filling a Guidance Gap: A Scientific Statement From the American Heart Association.Hypertension,DOI:https://doi.org/10.1161/HYP.0000000000000195
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AHA#
32
感谢分享!
57
学习到了
61
已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读已读
68
谢谢
56