JAMA子刊:长期使用质子泵抑制剂对癌症患者的潜在安全性
2021-06-20 MedSci原创 MedSci原创
质子泵抑制剂(缩写为PPI)或称氢离子阻断剂,是一种抑制氢离子泵的药物,这种药物对于减少胃酸分泌的作用是显著且长效的,是现今减少胃酸分泌第二强效的药物,仅次于钾离子竞争性胃酸抑制剂(P-CAB)。
质子泵抑制剂(缩写为PPI)或称氢离子阻断剂,是一种抑制氢离子泵的药物,这种药物对于减少胃酸分泌的作用是显著且长效的,是现今减少胃酸分泌第二强效的药物,仅次于钾离子竞争性胃酸抑制剂(P-CAB)。
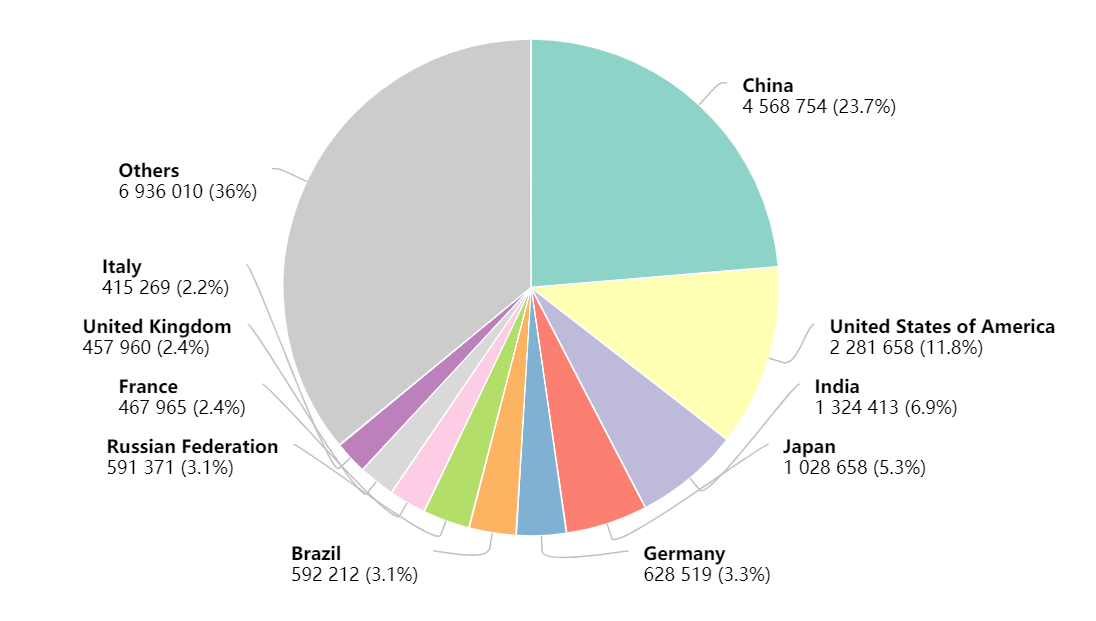
一直以来,PPI是许多胃肠道疾病的一线治疗,广泛用于治疗急、慢性消化系统酸相关性疾病,包括胃食管反流病(GERD)、消化性溃疡、上消化道出血及相关疾病。质子泵抑制剂(PPI)是最广泛的处方药之一,自上世纪80年代起,质子泵抑制剂的发现已成为美国第三大处方药。

近日,发表在JAMA Netw Open杂志的一项研究,评估了PPI使用的普遍性,同时探索与PPI相关的因素,并关注接受酪氨酸激酶抑制剂(TKI)、CPI和卡培他滨的患者。这项横断面研究于2020年6月15日至19日和6月22日至26日在4个法国综合癌症中心进行。研究人员收集了在咨询时或在即日病房就诊的癌症患者的数据。最终纳入872名癌症患者,其中566 名女性 (64.9%) 和 306 名男性 (35.1%),年龄中位数为63岁。
结果显示,大多数使用PPI的患者都是定期使用(163名患者[71.1%]),正常剂量(154名患者[67.2%]),用于上腹痛(114名患者[50.0%])、胸骨后疼痛(32名患者[14.0%])、已证实的食道或胃溃疡(18名患者[8.0%])或胃保护(34名患者[15.0%])。
在单变量和多变量分析中,与 PPI 使用相关的因素是年龄,激素治疗,癌症转移期和肿瘤部位。同时,使用PPI的流行率随癌症治疗的不同而不同。在服用TKIs和PPI的20名患者中,有16人报告长期使用PPI,主要用于上腹痛。
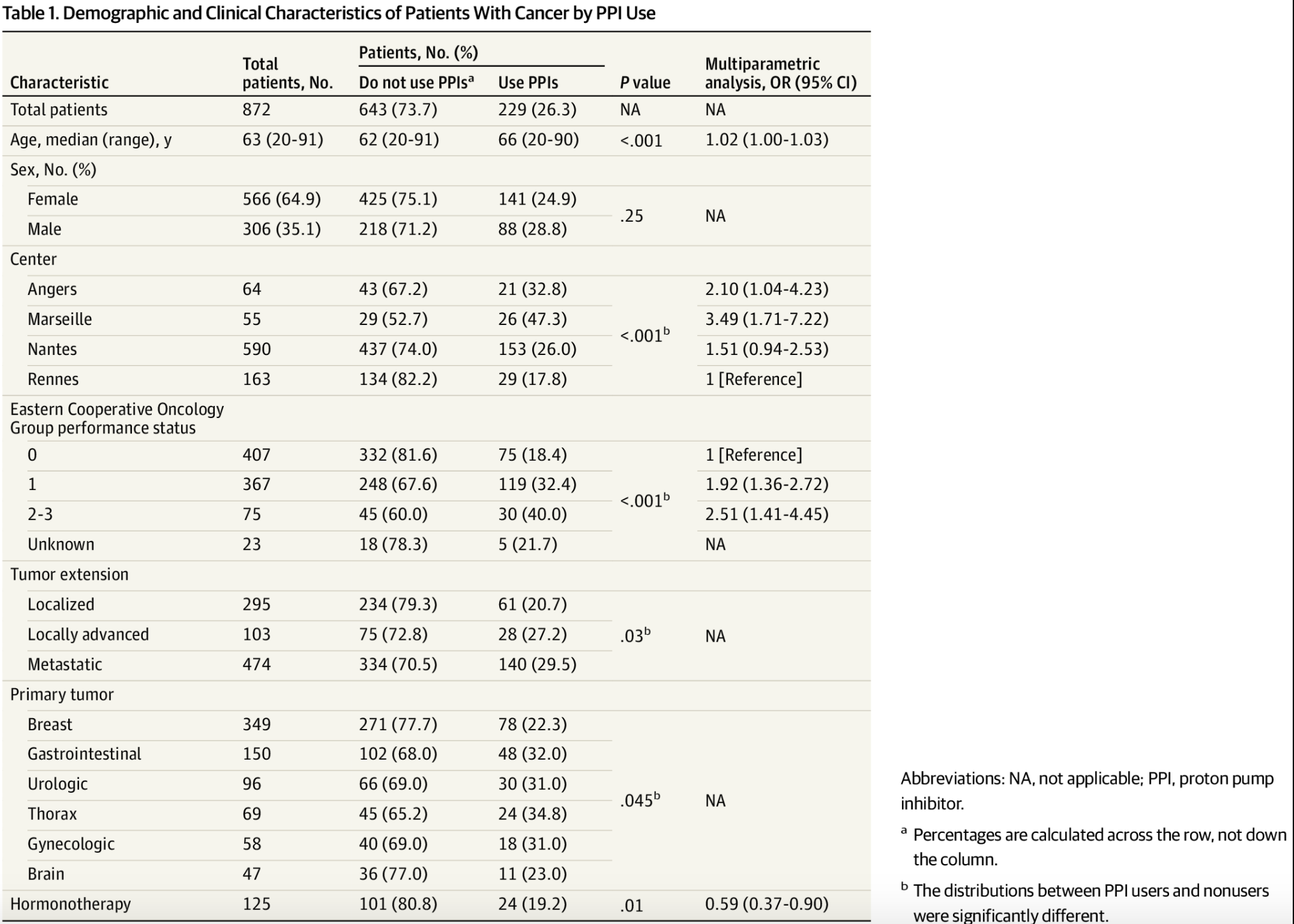
使用 PPI 的癌症患者的人口统计学和临床特征
另外,观察134名患者在与PPI一起使用时疗效下降的药物,有39名(29%)同时服用处方药:卡培他滨(21名患者中的5名)、舒尼替尼(9名患者中的5名)、卡博赞替尼(3名患者中的2名)、帕唑帕尼(5名患者中的1名)、吉非替尼(1名1名)、厄洛替尼(2名1名)和索拉非尼(3名1名),以及90名患者中有23名接受CPI。
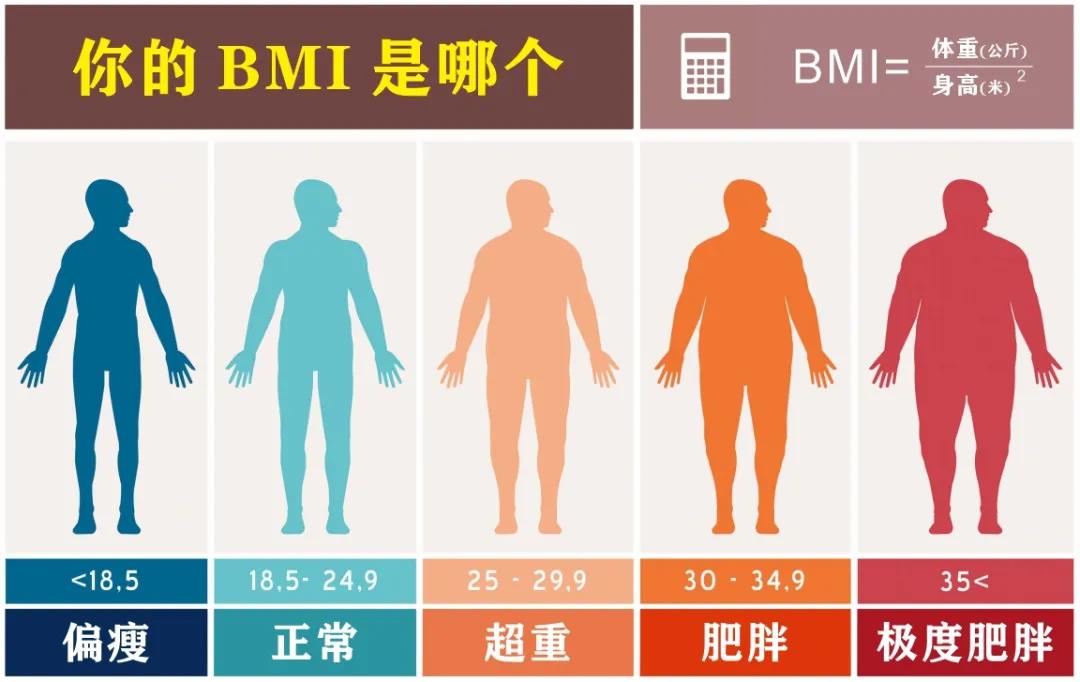
总之,在这项横断面研究中,超过四分之一的患者(主要是 PS 较差的老年人)使用 PPI。长期使用 PPI 的癌症患者可能会出现各种合并症,如肾功能障碍、贫血、感染或低镁血症。此外,间接的药物相互作用(例如,TKIs和卡培他滨的吸收率降低和肠道微生物组的变化)与其中一些药物的生存获益降低有关。
因此,应积极识别和替代 PPI。在胃灼热或上腹痛的情况下,应使用抗酸剂;H2拮抗剂是另一种选择。TKI 必须在 H2 拮抗剂之前 2 小时或之后 10 小时服用。如果强制使用 PPI,则必须在早上 PPI 前 2 小时给予 TKI,或与酸性饮料一起给予。对于服用 CPI 的患者,使用抗酸剂是最好的选择。
原始出处
Jean-Luc Raoul, MD, PhD1; Catherine Guérin-Charbonnel, PhD2; Julien Edeline, MD, PhD3; et al.Prevalence of Proton Pump Inhibitor Use Among Patients With Cancer.JAMA Netw Open. 2021;4(6):e2113739. doi:10.1001/jamanetworkopen.2021.13739
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#长期使用#
44
学习的
49
#抑制剂#
37
#质子泵#
48
#癌症患者#
37
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
46