胆管癌治疗困境有望打破,多款创新疗法迎来胆管癌治疗新希望!
2022-08-14 Dr HopeNoah 厚朴方舟
虽然胆管癌的恶性程度较高,但手术治疗、质子治疗、靶向治疗、免疫治疗等创新疗法的出现为胆管癌患者提供了新的选择,也为患者带来了新的希望。
胆管癌是一种恶性程度极高的肿瘤,多年来胆管癌的死亡率一直居高不下,如何提高胆管癌的预后效果,延长患者的生存期十分关键。近年来,随着手术治疗、质子治疗、靶向治疗等多种创新疗法的出现,胆管癌的治疗也迎来了新的方向。
胆管癌的根治手段:手术治疗
目前根治性手术切除是治疗胆管癌的主要手段,也是胆管癌患者获得长期生存的重要方法。
根据肿瘤发生部位不同,胆管癌可分为肝内胆管癌、肝门部胆管癌和远端胆管癌,三种胆管癌的手术方式也有一定的差异,但无论是哪种胆管癌,都可以在手术切除后获得良好的预后。
-
肝内胆管癌:肝内胆管癌的手术方式与原发性肝癌类型,均采用肝切除术治疗。由于肝内胆管癌往往不伴有肝硬化,肝脏储备功能良好,因此积极采用根治性肝切除术可以让患者获得长期的生存。
-
肝门部胆管癌:肝门部胆管癌手术涉及门静脉、肝动脉、胆管三个管道系统,被称为普外科手术的珠穆朗玛峰。同时,由于肿瘤发现时多已侵犯肝门部重要结构,肝门部胆管癌手术切除率较低,但是,手术切除的效果显著,因此对于肝门部胆管癌患者仍应优选手术治疗。
-
远端胆管癌:手术切除是远端胆管癌唯一可以获得根治的手段,与肝门部或肝内胆管癌相比,远端胆管癌的可切除率最高。远端胆管癌手术常采用胰十二指肠切除术(Whipple's手术)。
另外,新辅助治疗及转化治疗的出现可以显著提高胆管癌手术的可切除率,让一些原本无法完全切除肿瘤的胆管癌患者有望实现根治,进一步提高患者的预后效果。
-
2015年的一项研究揭露,针对肝门部胆管癌或远端胆管癌,采用新辅助放化疗治疗后,R0 切除率达到 80.9%[1]。
-
2018年的一项研究表明,对于初始不可切除的局部晚期胆管癌采用放化疗后,73.3%的患者被判定为可切除胆管癌,并接受了根治性肝切除术(60%的患者实现了R0切除),在接受手术切除的患者中,中位生存时间为37个月,1 年、2 年和 5 年生存率分别为 80.8%、70.7% 和 23.6%[2]。

▲图源:参考来源[2]
总而言之,胆管癌治疗的首选手段仍然是手术切除,但是胆管癌尤其是肝门部胆管癌手术难度大、危险性高,对医生技术水平要求极高,并非所有医院都可开展。因此,胆管癌患者选择手术经验丰富的专家治疗十分关键。
肝内胆管癌的重要放疗手段:质子治疗
肝内胆管癌是常见的胆管癌类型,也是常见的肝脏恶性肿瘤之一,放射治疗是肝内胆管癌主要的治疗手段。质子治疗作为一种新兴的放疗手段,可以将更多的放射剂量集中于病灶部位,治疗的效果更加显著且对人体正常组织造成的伤害更小,有效降低了放疗对人体造成的毒副作用。
2018年一项前瞻性II期研究报道了高剂量适形质子治疗胆管癌的突出效果。研究结果显示,质子治疗肝内胆管癌的2年肿瘤局部控制率和总生存率分别为94%和47%[3]。

▲图源:NIH
胆管癌的创新疗法:靶向治疗
由于胆管癌在早期多无特异性症状,患者常在确诊时即为晚期,失去手术机会,药物治疗是主要的治疗手段。此前,化疗是晚期胆管癌的主要手段,但是化疗的效果不佳,且常常出现耐药。
自2020年4月,首款胆管癌靶向药Pemazyre(培米替尼)获美国 FDA 批准上市后,胆管癌的靶向治疗迎来了突破性进展,为胆管癌患者提供了新的治疗选择。
▲图源:FDA
目前,已有三款胆管癌靶向药物获批于临床:
-
Pemazyre:2020年4月,Pemazyre率先获得美国FDA批准,用于治疗先前已接受过治疗、存在FGFR2融合或重排、不能手术切除的局部晚期或转移性胆管癌患者;2021年3月日本厚生劳动省(MHLW)批准[4]。推荐阅读:重磅!胆管癌首款靶向药已在日本各大医院上架,延长生存期近3倍
-
Truseltiq:2021年6月,美国食品和药物管理局(FDA)已加速批准Truseltiq(infigratinib),用于治疗先前接受过治疗、携带FGFR2融合或重排的局部晚期或转移性胆管癌(CCA)患者[5]。
-
Tibsovo:2021年8月,FDA批准靶向治疗药物Tibsovo(ivosidenib)用于治疗携带IDH1突变的局部晚期或转移性胆管癌成人患者,成为首个获批用于治疗这一患者群体的靶向疗法[6]。
有望改善晚期胆管癌效果:免疫疗法
相比进展颇丰的胆管癌靶向治疗,胆管癌的免疫治疗目前仅有一款药物的效果显著优于传统疗法。
2021年11月,针对胆管癌一线免疫治疗的TOPAZ-1 3期试验结果公布,此次数据表明,抗PD-L1疗法Imfinzi(英飞凡,通用名:durvalumab,度伐利尤单抗)联合化疗显著延长了胆管癌患者的总生存期(OS)、无进展生存期(PFS),显著提高有效率(ORR)[7]。
今年更新的第1版胆管癌NCCN指南中新增Imfinzi+吉西他滨+顺铂作为胆管癌的一线治疗(2B类证据)和二线治疗方案(2B类证据)[8]。
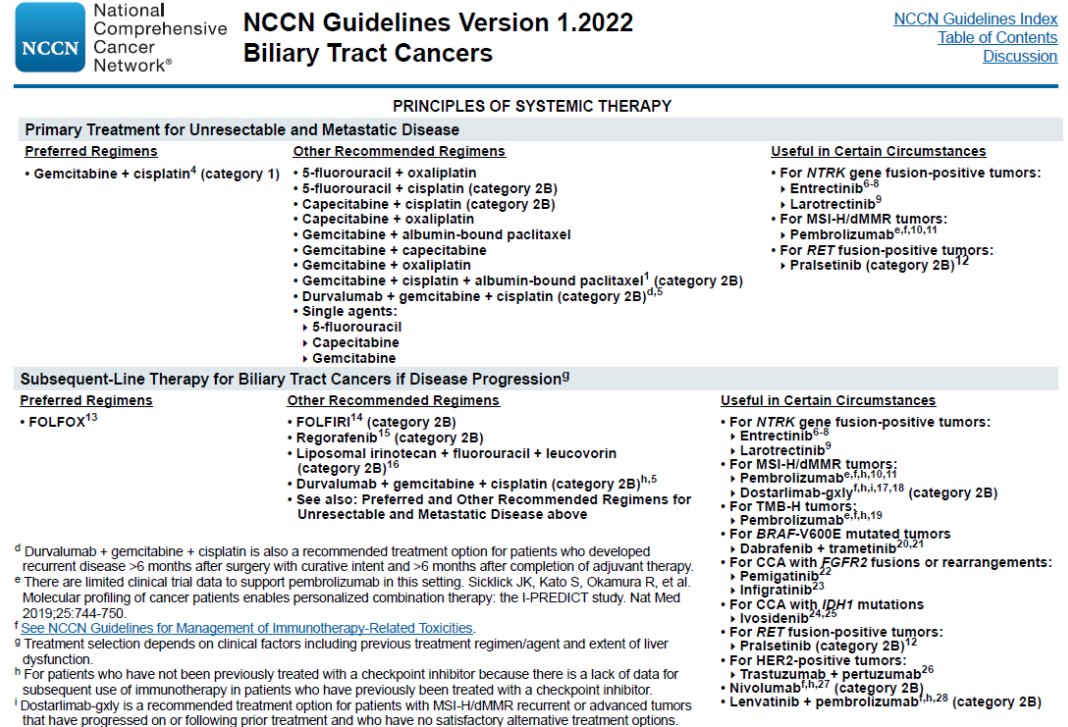
▲图源:参考来源[8]
虽然胆管癌的恶性程度较高,但手术治疗、质子治疗、靶向治疗、免疫治疗等创新疗法的出现为胆管癌患者提供了新的选择,也为患者带来了新的希望。相信随着临床研究的深入开展,将会有越来越多的创新疗法获批于临床,让更多胆管癌患者受益。
美国麻省总医院是美国最大的胆道疾病治疗医院之一,也是美国首屈一指的胆管癌治疗医院。在《美国新闻与世界报道》发布的2021-22年度最佳医院排名中, 麻省总医院排名前五。
在放射治疗领域,麻省总医院是美国最早的胃肠道放射肿瘤专科,也是国际公认的胃肠放射肿瘤专科领导者,该科室拥有世界先进的质子治疗、可以专门用于术中放射治疗的技术、4DCT扫描等放疗技术;在研究领域,麻省总医院积极参与胆管癌相关的临床试验和研究,可以尽快为患者带来有希望的新疗法。
参考来源:
[1]A review of current adjuvant and neoadjuvant systemic treatments for cholangiocarcinoma and gallbladder carcinoma
https://hrjournal.net/article/view/4387#B55
[2]Sumiyoshi T, Shima Y, Okabayashi T, Negoro Y, Shimada Y, Iwata J, Matsumoto M, Hata Y, Noda Y, Sui K, Sueda T. Chemoradiotherapy for Initially Unresectable Locally Advanced Cholangiocarcinoma. World J Surg. 2018 Sep;42(9):2910-2918. doi: 10.1007/s00268-018-4558-1. PMID: 29511872.
[3]Badiyan SN, Hallemeier CL, Lin SH, Hall MD, Chuong MD. Proton beam therapy for gastrointestinal cancers: past, present, and future. J Gastrointest Oncol 2018;9(5):962-971.
[4] インサイト・コーポレーション、ペマジール:registered:(ペミガチニブ)の国内製造販売承認取得を発表
https://prtimes.jp/main/html/rd/p/000000004.000060544.html
[5] BridgeBio Pharma’s Affiliate QED Therapeutics and Partner Helsinn Group Announce FDA Approval of TRUSELTIQTM (infigratinib) for Patients with Cholangiocarcinoma.
[6] Servier Announces FDA Approval of TIBSOVO:registered: (ivosidenib tablets) in IDH1-Mutated Cholangiocarcinoma
https://www.prnewswire.com/news-releases/servier-announces-fda-approval-of-tibsovo-ivosidenib-tablets-in-idh1-mutated-cholangiocarcinoma-301363055.html
[7] Imfinzi plus chemotherapy significantly improved overall survival in 1st-line advanced biliary tract cancer in TOPAZ-1 Phase III trial at interim analysis
https://www.astrazeneca.com/content/astraz/media-centre/press-releases/2021/imfinzi-improved-survival-in-biliary-tract-cancer.html
[8]2022.v1《NCCN肿瘤学临床实践指南:胆管癌》
- END -
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#新希望#
51
#困境#
61
#创新#
52
#新疗法#
65
#胆管#
54