Eur Radiol:对于低风险局灶性前列腺癌,MRI上哪些征象提示肿瘤进展呢?
2021-02-04 shaosai MedSci原创
有些前列腺癌病灶处在进展低风险时,直接做手术有点不值当的,不做手术吧又有点不放心!那对于这样的前列腺癌,我们该拿它如何是好呢?
有些前列腺癌病灶处在进展低风险时,直接做手术有点不值当的,不做手术吧又有点不放心!那对于这样的前列腺癌,我们该拿它如何是好呢?
积极检测(AS)是当前局灶性低风险前列腺癌患者被推荐的指导方案。AS的目的主要是减少过度治疗的同时识别肿瘤进展,进展程度可控在可治愈性时间窗内。
多参数磁共振成像(mpMRI)检查现被作为AS方案中不可或缺的一部分。然而,随访观察主要基于联合前列腺特异抗原(PSA)、数字直肠检查和再分期活检等临床综合信息。该方案中有创性的活检方法使得部分患者对AS望而却步,而MRI扫描由于其无创性对有创性评估方法具有一定的替代作用。因此,mpMRI在AS随访方案中的角色越来越重要。不过,对评价影像学上进展征象的一致性却参差不齐。那么,找出一种具有可靠性的mpMRI评估方案的呼声越来越高。
近日,Eur Radiol上发表的一篇名为MRI-derived PRECISE scores for predicting pathologically-confirmed radiological progression in prostate cancer patients on active surveillance的论文通过建立接受积极监测(AS)的前列腺癌(PCa)患者前列腺癌影像学系列评估中变化(PRECISE)系统,明确PRECISE系统提示进展的预测价值及其与病理进展的相关性。
本研究纳入2011年至2018年间参加AS研究的295名PCa患者。在AS开始时首先进行基线多参数磁共振成像(mpMRI)以备活检。 两名分别拥有10年和13年经验的泌尿放射科医生对随访的mpMRI研究进行了前瞻性评估。 在最佳截断值4的临界值将患者PRECISE评分分为两组,并计算其灵敏度、特异性、阳性预测值和阴性预测值。基于联合MRI-US指导活检结果来建立ROC曲线,利用ROC 曲线下面积来评价诊断性能。利用Cox回归进行单变量分析评估基线时临床和mpMRI参数与AS疾病进展的相关性。

图. PRECISE评分1。PSA为4.53ng/ml的62岁男性患者。

图. PRECISE评分2。PSA为3.4ng/ml的72岁男性患者。
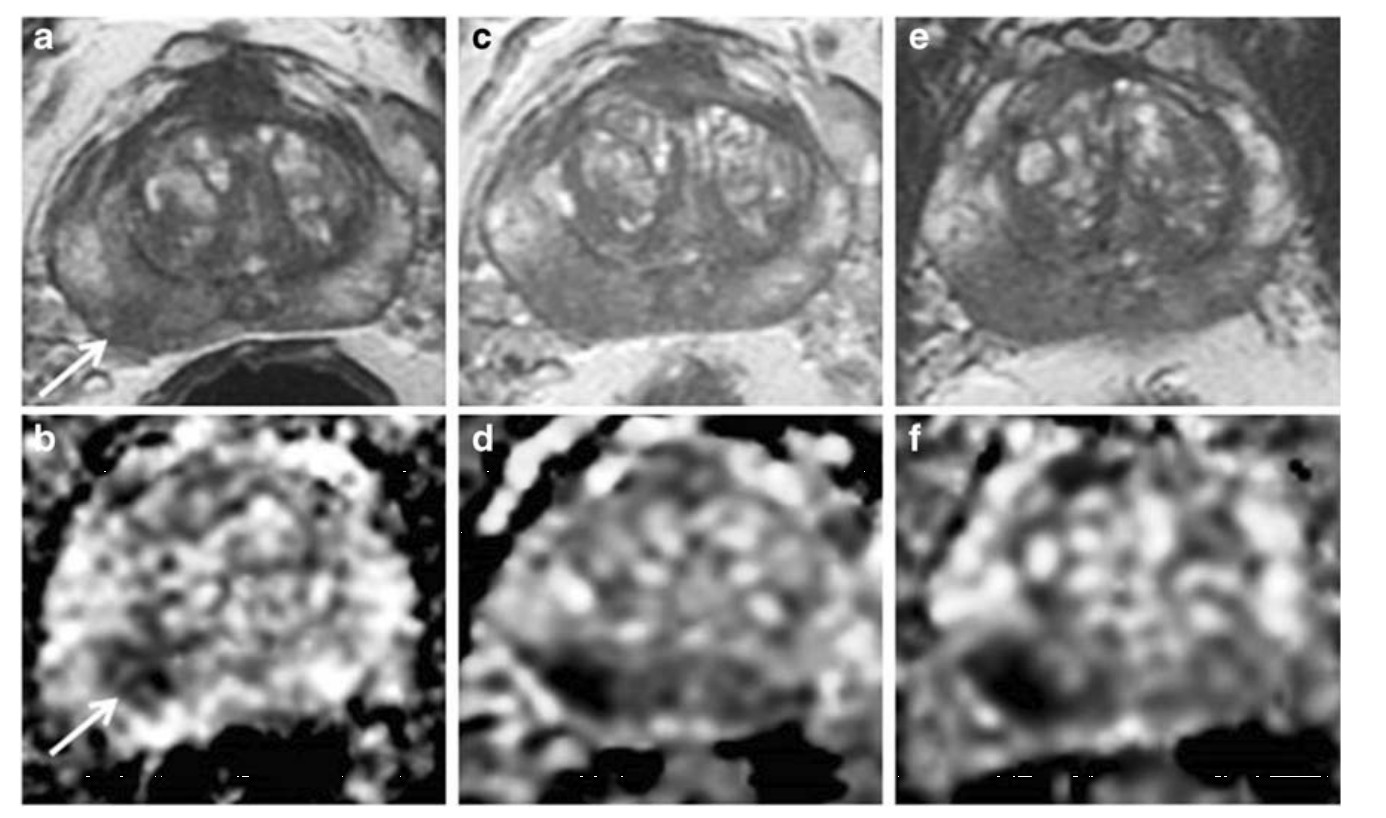
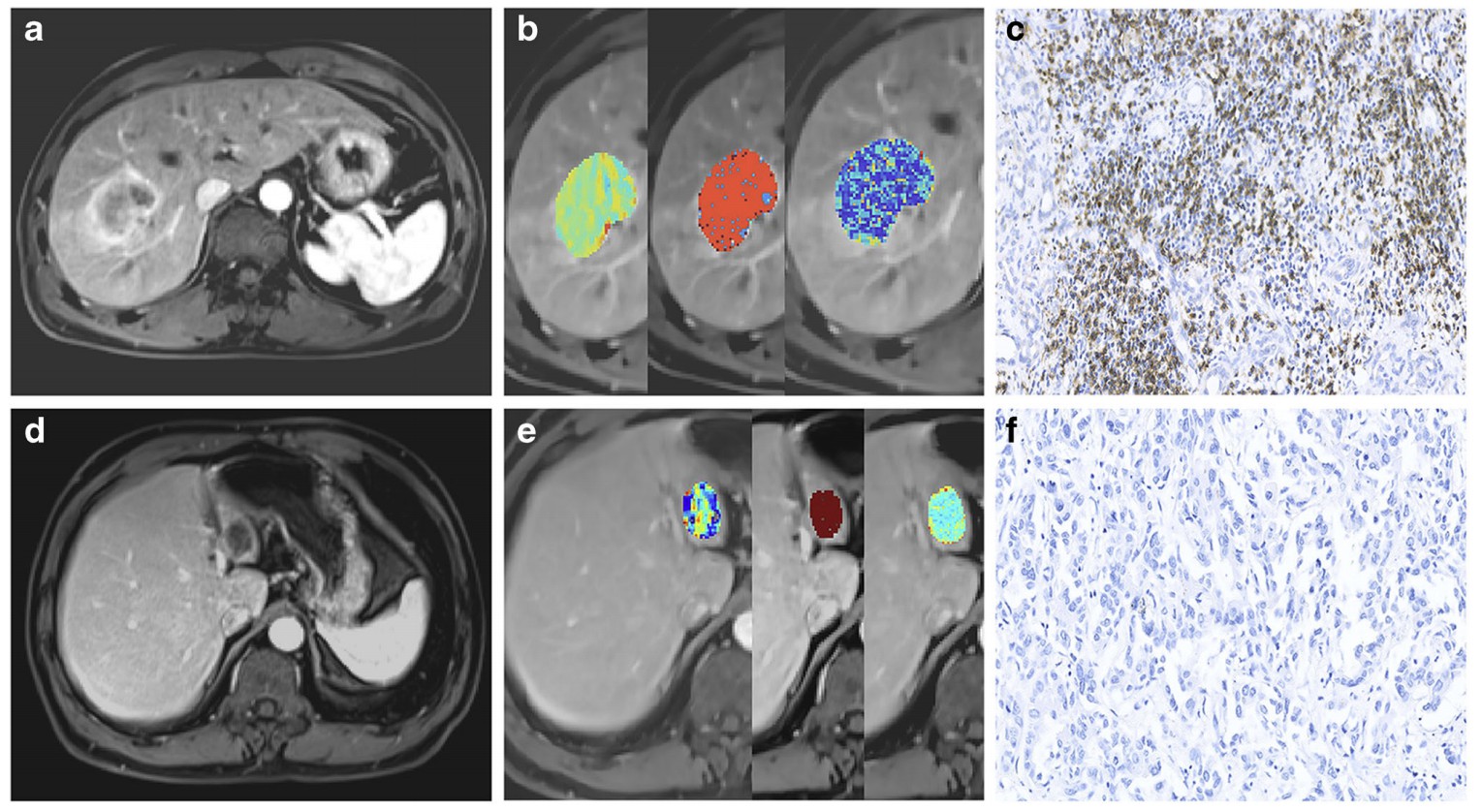
图. PRECISE评分4。PSA为3.09ng/ml的66岁男性患者。
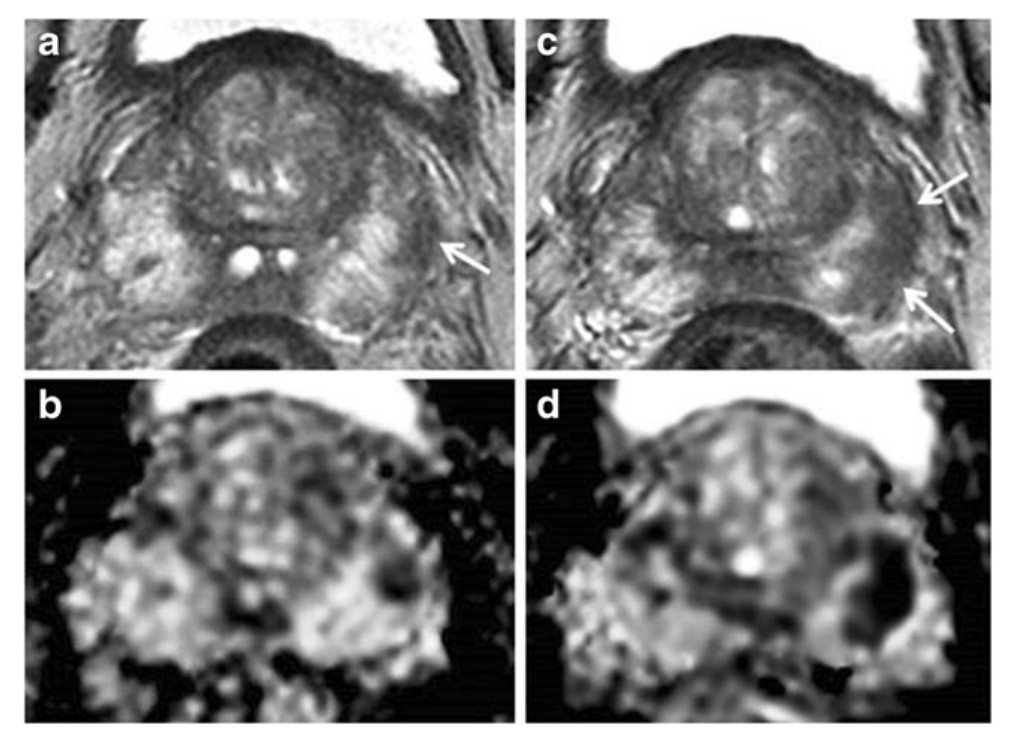
图. PRECISE评分5。PSA为5.1ng/ml的68岁男性患者。
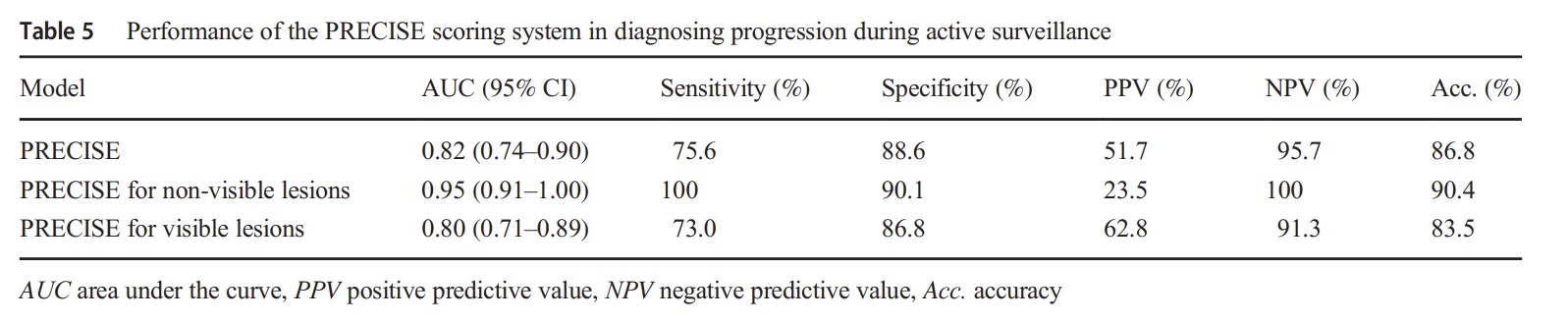
图. PRECISE评分系统在评价处在AS的前列腺癌患者的价值
在52个月的中位随访中,该队列的进展率为13.9%(41/295)。 临界值≥4时,Precise评分系统显示出预测AS进展的敏感性、特异性、PPV和NPV分别为0.76、0.89、0.52和0.96。 AUC为0.82(95%CI = 0.74-0.90)。 仅有前列腺特异性抗原密度(PSA-D)、李克特病灶评分和病灶大小是肿瘤进展的基线预测指标(均p <0.05)。
PRECISE评分系统对评估前列腺癌肿瘤进展具有良好诊断效能,其较高的NPV可能有助于减少AS患者所需的随访活检次数。
原始出处:
Iztok Caglic,Nikita Sushentsev,Vincent J Gnanapragasam,et al. MRI-derived PRECISE scores for predicting pathologically-confirmed radiological progression in prostate cancer patients on active surveillance.DOI:10.1007/s00330-020-07336-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


.jpg)







#肿瘤进展#
31
#局灶性#
44
厉害啦
90
涨知识
91
前列腺癌相关研究,学习了,谢谢梅斯
51