Blood:急性髓系白血病的新靶点——新型CDK9复合物!
2019-01-16 MedSci MedSci原创
中心点:CDK9与mTOR复合物胞内原件的不同部位结合,形成CDK9-mTOR样复合物(CTORC1和CTORC2)。CTORC1控制对白血病发生重要的基因的转录,而CTORC2调控mRNA的翻译。摘要:在急性髓系白血病(AML)中,mTOR信号的异常激活可导致存活优势,从而促进恶性表型。为了提高我们对mTOR信号激活因子的认识,鉴别新的治疗靶点,Elspeth M. Beauchamp等人通过蛋
CDK9与mTOR复合物胞内原件的不同部位结合,形成CDK9-mTOR样复合物(CTORC1和CTORC2)。
CTORC1控制对白血病发生重要的基因的转录,而CTORC2调控mRNA的翻译。
摘要:
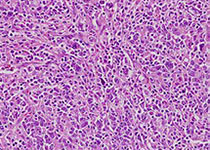
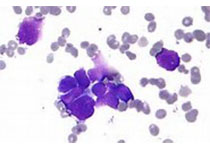
在急性髓系白血病(AML)中,mTOR信号的异常激活可导致存活优势,从而促进恶性表型。为了提高我们对mTOR信号激活因子的认识,鉴别新的治疗靶点,Elspeth M. Beauchamp等人通过蛋白组学分析来寻找mTOR复合物特异的相互作用体。
研究人员发现细胞周期蛋白依赖性激酶9 (CDK9)是mTOR复合物支架蛋白(mLST8)的一种新的结合伴侣。研究人员并证实CDK9在细胞质和细胞核中以不同的mTOR样复合物(CTOR)形式存在。在细胞核中,CDK9与RAPTOR和mLST8结合形成CTORC1,促进对白血病发生至关重要的基因的转录。在细胞质中,CDK9与RICTOR、SIN1和mLST8结合形成CTORC2,通过LARP1和rpS6的磷酸化调控mRNA的翻译。
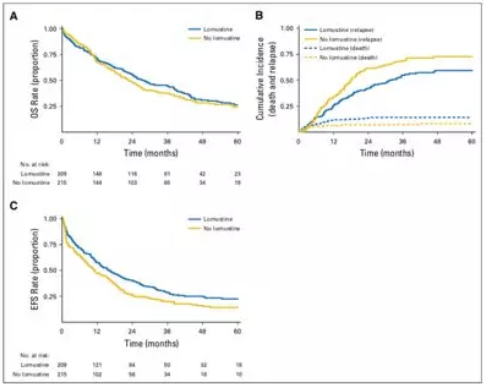
用药物靶向CTORC复合物,在体外可抑制原始人AML祖细胞的生长,在AML异种移植体体内引发强烈的抗白血病反应。
综上所述,本研究提示CDK9可与mTOR复合物结合从而激活mTOR信号,CDK9的mTOR样复合物(CTORC1和CTORC2)或可作为抗白血病治疗的新的药物靶点。
Elspeth M. Beauchamp, et al.Identification and targeting of novel CDK9 complexes in acute myeloid leukemia.Blood 2018 :blood-2018-08-870089; doi: https://doi.org/10.1182/blood-2018-08-870089
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#复合物#
28
#髓系白血病#
23
#CDK#
22
#新靶点#
17
好
69
学习了长知识
61
学习了新知识
75
学习了长知识
63
学习了新知识
50
学习了长知识
21