网络导向型SOCS3基因的循环CD4+T细胞甲基化特征与肺动脉高压患者的血流动力学之间的关系
2022-08-14 刘少飞 MedSci原创
DNA甲基化特征的改变与脂质代谢、不完全渗透和促炎症途径有关,这些都与PAH的发病机制有密切关系。然而,以前没有研究调查PAH患者的DNA甲基化变化及其与血流动力学参数的潜在联系。
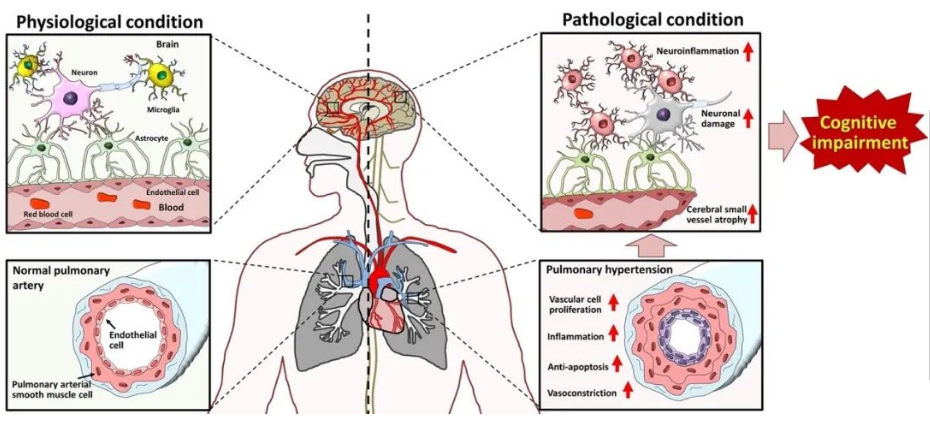
肺动脉高压(PAH)是一种高发病率的心肺疾病,尽管有血管扩张剂和其他疗法,但与寿命缩短有关。在临床试验和实践中,不同的PAH亚组和个体患者的治疗反应是不同的。这是因为PAH的血管和心脏重塑的分子基础具有高度的异质性,目前还没有建立起具体的生物标志物。PAH的复杂性质表明,主要由DNA甲基化引导的表观遗传敏感机制是肺血管逐渐重塑的关键因素,导致血管阻力增加和随之而来的右心室重塑。DNA甲基化是一种由DNA甲基转移酶介导的共价酶修饰,它在位于5′-CpG-3′二核苷酸中的胞嘧啶碱基的5′碳上添加一个或多个甲基。后者在启动子的CpG岛(CGI)区域最为丰富,可以在转录水平上调节基因的表达速度。一般来说,进入CGI-启动子区域的DNA甲基化等级与基因活性之间存在反比关系,对于这种情况,DNA高甲基化容易使基因表达沉默,而DNA低甲基化在转录上更容易被允许。以前的临床证据显示,DNA甲基化特征的改变与脂质代谢、不完全渗透和促炎症途径有关,这些都与PAH的发病机制有密切关系。然而,以前没有研究调查PAH患者的DNA甲基化变化及其与血流动力学参数的潜在联系。
因此,我们利用大型CLEOPAHTRA试验(NCT04282434 at clinicaltrials.gov)对表型良好的患者进行测试,假设PAH患者凭借循环CD4+T细胞DNA甲基化特征与健康对照组不同,反过来,这可能与受影响患者的表型和预后有关。我们研究的目的是对患者来源的CD4+T细胞甲基化特征进行网络分析,以发现PAH患者在诊断时或早期随访时的新的潜在致病机制。尽管单核细胞和骨髓细胞在PAH反应中的作用众所周知,但CD4+T细胞一直未被充分研究,目前在实验和临床研究中都被视为肺血管重塑的关键角色。此外,根据我们以前的经验,我们选择循环的CD4+T细胞是因为它们在捕捉DNA甲基化特征和反映潜在临床意义的分子途径方面的效用。在此,我们进行了一项新的研究计划,整合了临床表观遗传学和网络医学分析方法,以推进PAH的精准医疗。这项研究的结果具有直接的转化潜力,从生物标志物的发现和验证到治疗目标的确定,可以在未来的调查中进一步研究。
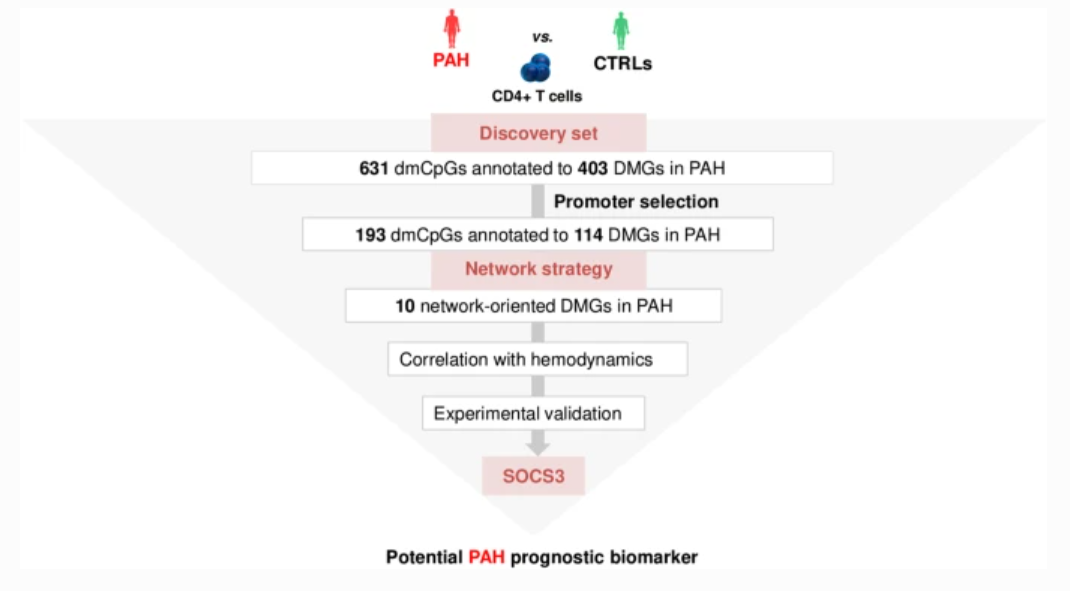
减少的代表性亚硫酸氢盐测序(RRBS)分析显示了N=631个不同甲基化的CpG位点,这些位点被注释为N=408个基因(DMGs),这些基因分离自PAH患者与健康对照组(CTRLs)的循环CD4 T细胞中。启动子限制网络分析建立了PAH子网络,包括5个枢纽DMGs(SOCS3、GNAS、ITGAL、NCOR2、NFIC)和5个非枢纽DMGs(NR4A2、GRM2、PGK1、STMN1、LIMS2)。功能分析显示,SOCS3基因是富集PAH子网络的前十条重要途径中重复出现最多的,包括生长激素受体和白细胞介素-6信号传导。相关分析显示,每个网络导向的DMG的启动子甲基化水平都与血液动力学参数单独相关。特别是SOCS3低甲基化与右心房压力(RAP)呈负相关,与心脏指数(CI)呈正相关(|r|≥0.6)。在PAH患者与CTRLs的外周血单核细胞中发现SOCS3、ITGAL、NFIC、NCOR2和PGK1 mRNA水平明显上调(qRT-PCR)(P≤0.05)。通过免疫印迹法,证实PAH患者与CTRLs相比,SOCS3蛋白明显上调(P<0.01)。这是第一个以网络为导向的研究,它整合了循环CD4 T细胞DNA甲基化特征、血液动力学参数和验证实验,对PAH患者进行首次诊断或早期随访。我们的数据表明,SOCS3基因可能参与PAH的发病机制,并作为潜在的预后生物标志物。
参考文献:
Benincasa G, Maron BA, Affinito O, D'Alto M, Franzese M, Argiento P, Schiano C, Romeo E, Bontempo P, Golino P, Berrino L, Loscalzo J, Napoli C. Association Between Circulating CD4+ T Cell Methylation Signatures of Network-Oriented SOCS3 Gene and Hemodynamics in Patients Suffering Pulmonary Arterial Hypertension. J Cardiovasc Transl Res. 2022 Aug 12. doi: 10.1007/s12265-022-10294-1. Epub ahead of print. PMID: 35960497.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CD4#
44
#血流动力#
51
#动脉高压#
0
#肺动脉高压患者#
51
#CD4+#
36
#血流动力学#
37
#CD4+T细胞#
38