烟酰胺核苷酸转氢酶的逆反应促进 ROS 的产生并导致因肺动脉压力过高引起的右心室衰竭
2022-08-14 刘少飞 MedSci原创
在本期的《JACC: Basic to Translational Science》Müller等人对PAB小鼠模型进行了全面的描述,并提供了线粒体活性氧(mROS)的过度产生明显导致RV衰竭的证据。
右心室(RV)功能障碍是一个重要的预后预测因素,也是几个临床实体的终末期事件。为了应对压力负荷过大,右心室经历了一个渐进的重塑过程,通常分为两个阶段。在早期阶段,肥大反应伴随着收缩性能的增强而发生,保留了RV功能。然而,面对持续的血流动力学压力,这种适应性或补偿性肥大不能无限期地维持,并逐渐过渡到适应不良的状态,其特点是代谢功能紊乱、氧化应激、炎症、纤维化和肌细胞死亡的自我持续的有害循环,导致RV性能逐渐下降和潜在死亡。不幸的是,牵涉到适应不良的RV重塑的分子机制和因素还不是很清楚,有效治疗的希望在于研究出一种方法来打破这种RV故障轨迹的恶性循环。这一点更为重要,因为标准的左心衰竭治疗方法未能改善左心衰竭患者的功能和存活率;这种缺乏效率的情况往往归因于两个心腔不同的胚胎学、几何学和结构特性。慢性RV衰竭的基础和临床前研究依赖于不同的动物模型,包括肺动脉绑扎(PAB)模型,它具有解决直接RV治疗效果的优势。因此,大鼠和小鼠的PAB被认为是一个坚实的模型,对于它来说,可以应用不同程度的肺动脉收缩来诱导轻度到重度的RV功能衰竭,对于它来说,RV功能障碍的程度和进展可以通过无创成像技术来监测。
在本期的《JACC: Basic to Translational Science》Müller等人对PAB小鼠模型进行了全面的描述,并提供了线粒体活性氧(mROS)的过度产生明显导致RV衰竭的证据。研究利用携带烟酰胺核苷酸转氢酶(Nnt)基因自发功能缺失突变的C57BL/6J小鼠和它们的野生型对应小鼠(C57BL/6N),测试了Nnt的基因缺失可防止PAB引起的RV衰竭这一假设。NNT是一种位于线粒体内膜的核编码蛋白,它从烟酰胺腺嘌呤二核苷酸中产生烟酰胺腺嘌呤二核苷酸磷酸盐,从而供应抗氧化系统。有资料显示,NNT也可以反向操作,损害烟酰胺腺嘌呤二核苷酸的可用性,并提高mROS的过载,从而使NNT成为氧化还原平衡和下游结果的关键角色。Müller等人发现,与C57BL/6N小鼠相比,C57BL/6J小鼠在严重的PAB 4周后表现出较少的RV扩张和较高的三尖瓣环面收缩压值,以及没有肝静脉充血的迹象。虽然在心脏肥大和纤维化的程度方面没有看到明显的变化,但在PAB操作的C57BL/6J小鼠中,RV结构和功能的这种明显改善伴随着组织氧化性DNA损伤的减少,因此,凋亡细胞的数量也减少了。此外,用线粒体靶向抗氧化剂MitoTEMPO治疗PAB受试的C57BL/6N小鼠,改善了RV收缩功能和细胞存活率,证实了氧化作用在压力过载引起的RV衰竭中的因果作用。
这些结果反映了2015年Nickel等人所获得的结果,显示横向主动脉收缩-左心室(LV)的病理代谢需求和肥大使NNT切换到促氧化的反向模式。事实上,与本期报道的结果相似,C57BL/6N小鼠在主动脉横向收缩6周后,左心室衰竭的发展加剧,表现为氧化应激和纤维化增加,左心室射血分数受损,死亡率增加;而用mROS清除肽治疗后,情况有所缓解。
总的来说,这些研究很重要,因为它们提供了额外的证据,强调氧化应激是左心室和右心室衰竭发展和进展的一个共同机制。这些研究补充了最近的研究结果,即在各种左心衰竭或右心衰竭的动物模型中,抑制聚(二磷酸腺苷-核糖)聚合酶-1可通过中断代谢、氧化性DNA损伤和炎症干扰的恶性循环而起到保护心脏的作用。即使到目前为止,旨在预防或减少氧化应激的治疗策略(抑制黄嘌呤氧化酶、服用N-乙酰半胱氨酸等)在很大程度上未能改善心力衰竭患者的预后,也不能放弃针对它的想法。此外,虽然RV和左心室在很多方面都有不同,但这些研究支持这样的观点:一方的新治疗进展可能对另一方有益。
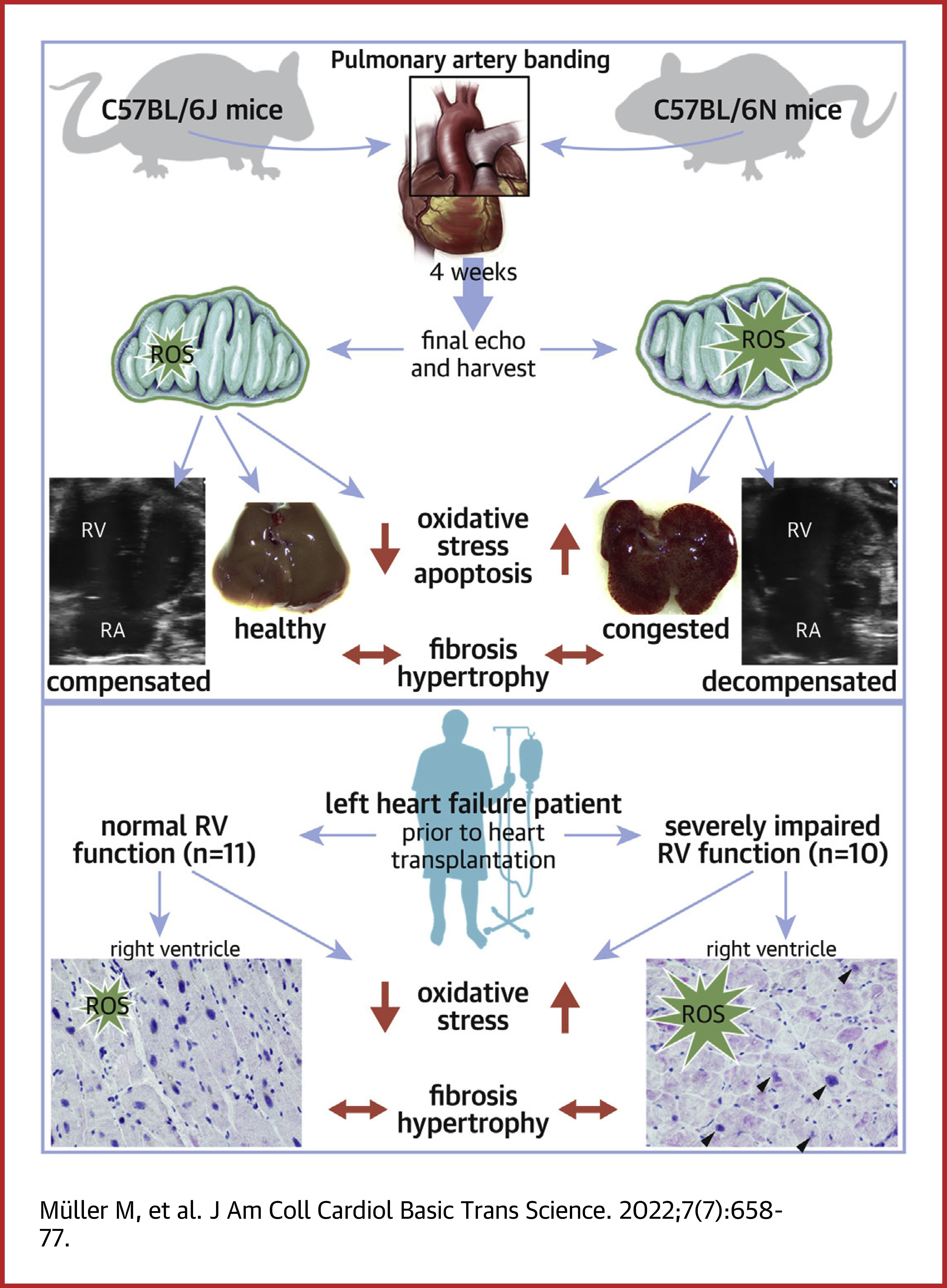
这项研究产生的另一个耐人寻味的观点是,针对RV纤维化是改善RV功能的一个有价值的途径这一概念受到挑战。事实上,Müller等人表明,C57BL/6J小鼠的NNT缺乏可保护其免受严重的PAB诱发的RV功能障碍,而纤维化程度没有任何变化。同样,他们发现在扩张型心肌病患者中,收缩期RV功能正常或严重受损,RV胶原的积累并无不同。纤维化在RV衰竭中的作用仍然是一个正在讨论的问题。一方面,纤维化被认为是限制心肌细胞过度伸展和保护RV形状的适应性反应的一部分。尽管细胞外基质成分的积累超过一定的阈值无疑会导致RV衰竭,但质的变化可能比量的变化更有害。事实上,具有不同机械和功能特性的各种基质蛋白的相对数量的变化可能会促使功能衰退。在严重的RV功能障碍的大鼠中,记录了胶原蛋白I/III比例增加的研究结果有助于这种方式。
最后,考虑到慢性氧化应激和炎症相互之间以及与RV功能障碍的演变密切相关,与两种菌株中炎症细胞的招募以及促炎症因子的表达和释放相关的额外数据将产生关键信息。
总之,这些数据提供了新的证据,表明针对氧化应激可能限制适应不良的RV重塑。从更普遍的角度来看,该研究指出了考虑干预性研究的遗传背景的重要性,并对以前使用C57BL/6J品系研究对RV压力负荷的反应的研究提出了新的启示。
参考文献:
Lemay SE, Boucherat O, Bonnet S. Reverse Reaction of Nicotinamide Nucleotide Transhydrogenase Promotes ROS Production and Contributes to Right Ventricular Failure. JACC Basic Transl Sci. 2022 Jul 25;7(7):678-680. doi: 10.1016/j.jacbts.2022.03.015. PMID: 35958692; PMCID: PMC9357571.
Müller M, Bischof C, Kapries T, Wollnitza S, Liechty C, Geißen S, Schubert T, Opacic D, Gerçek M, Fortmeier V, Dumitrescu D, Schlomann U, Sydykov A, Petrovic A, Gnatzy-Feik L, Milting H, Schermuly RT, Friedrichs K, Rudolph V, Klinke A. Right Heart Failure in Mice Upon Pressure Overload Is Promoted by Mitochondrial Oxidative Stress. JACC Basic Transl Sci. 2022 Jul 6;7(7):658-677. doi: 10.1016/j.jacbts.2022.02.018. PMID: 35958691; PMCID: PMC9357563.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动脉压#
42
#烟酰胺核苷#
48
#核苷酸#
45
太好的内容了,学习了!!!
35
#ROS#
47
#肺动脉压#
35
#右心室#
38