JAHA:细菌性心内膜炎微生物病因的时间变化、患者特征和死亡率
2022-08-13 MedSci原创 MedSci原创
这项全国性的研究表明,金黄色葡萄球菌是IE最常见的微生物病因,其次是链球菌和肠球菌。金黄色葡萄球菌IE患者的医院死亡率最高。
细菌性心内膜炎(IE)病原体的监测是了解IE的关键,然而来自大型队列的数据是较少。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员的目的是根据2010-2017年期间IE患者的微生物病因来评估时间变化、患者特征、住院和长期死亡率。

研究人员通过链接丹麦全国的登记中心确定了所有首次IE患者。根据微生物原因评估住院死亡率和长期死亡率,并分别使用多变量调整logistic回归分析和Cox比例风险分析进行了比较。
该研究共纳入了4123例患者。金黄色葡萄球菌是最常见的病因(28.1%),其次是链球菌(26.0%)、肠球菌(15.5%)、凝固酶阴性葡萄球菌(6.2%)和“其他微生物”(5.3%)。血培养阴性的IE占18.9%。在研究期间,血液培养阴性IE的比例有所下降,而没有看到任何微生物原因有显著的变化。与其他原因相比,肠球菌患者年龄更大,更常接受了人工心脏瓣膜。
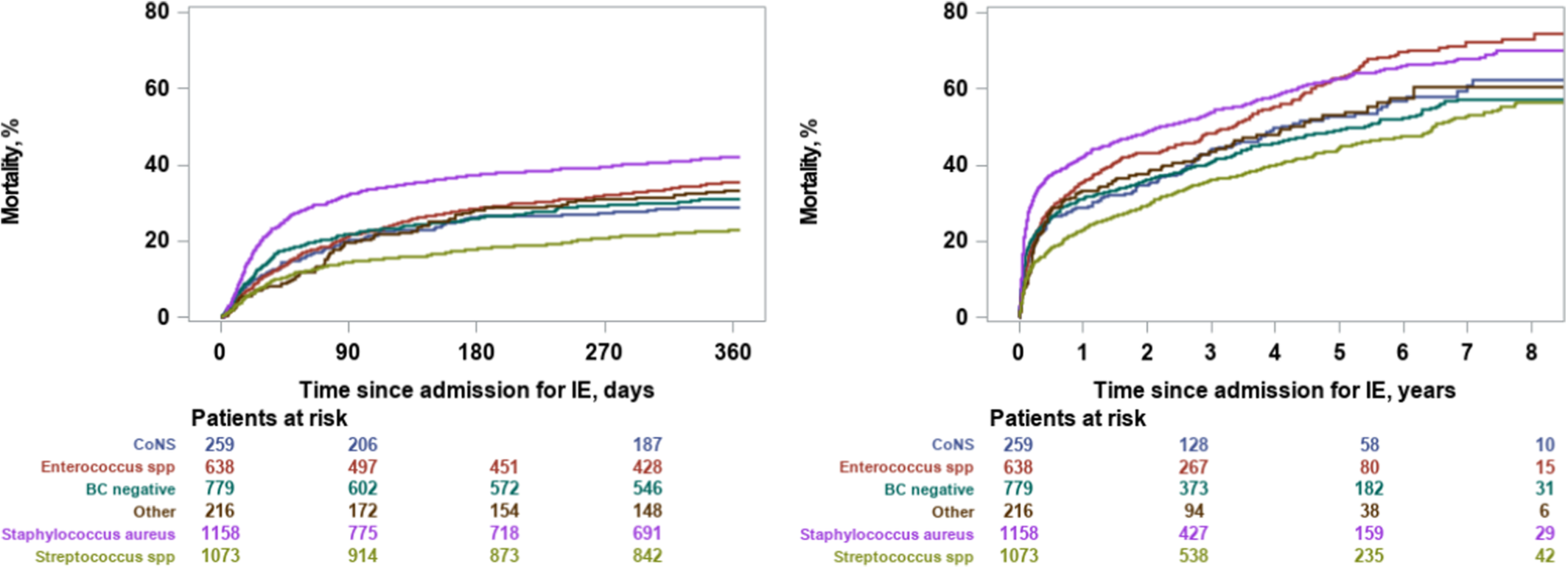
对于类链球菌IE,患者住院和长期死亡率(中位随访时间为2.3年)分别为11.1%和58.5%。与链球菌类IE相比,以下原因与较高的医院死亡率相关:金黄色葡萄球菌类IE(比值比[OR]为3.48[95%CI为2.74-4.42])、肠球菌类IE(OR为1.48[95%CI为1.11-1.97])、凝固酶阴性葡萄球菌类IE(OR为1.79[95%CI为1.21-2.65])、“其他微生物原因”IE(OR为1.47[95%CI为0.95-2.27])和血培养阴性IE(OR为1.99[95%CI为1.52-2.61]);以下原因与出院后较高的死亡率相关(中位随访时间为2.9年):金黄色葡萄球菌IE(风险比[HR]为1.39[95%CI为1.19-1.62])、肠球菌IE(HR为1.31[95%CI为1.11-1.54])、凝固酶阴性葡萄球菌IE(HR为1.07[95%CI为0.85-1.36])、“其他微生物原因”IE(HR为1.45[95%CI为1.13-1.85])和血液培养阴性IE(HR为1.05[95%CI为0.89-1.25])。
由此可见,这项全国性的研究表明,金黄色葡萄球菌是IE最常见的微生物病因,其次是链球菌和肠球菌。金黄色葡萄球菌IE患者的医院死亡率最高。
原始出处:
Lauge Østergaard.et al.Temporal Changes, Patient Characteristics, and Mortality, According to Microbiological Cause of Infective Endocarditis: A Nationwide Study.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.122.025801
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#微生物#
57
#内膜#
44
#AHA#
29
#心内膜炎#
57
#患者特征#
43