Nature:全新发现一种重要的癌症免疫治疗新方法:Gasdermin E
2020-03-23 佚名 生物通
近期来自波士顿儿童医院发现了癌症免疫疗法的另外一种新武器,可以在更多的癌症类型中发挥作用。这种方法利用人体内免疫反应重新激活称为Gasdermin E的基因,这种基因在许多类型的癌症中均被抑制。
这个在大多数肿瘤组织中沉默或突变的有效抑癌基因可以重新打开,引发靶向肿瘤的强大免疫攻击。

科学家们发现,肿瘤已经找到防止免疫系统攻击它们的各种方法。就医学而言,我们可以通过癌症免疫疗法进行了反击,其中主要方法是使用检查点抑制剂,这是一种有助于免疫系统将癌细胞识别为异物的药物。CAR-T细胞疗法是另一种方法,可以直接改造人们的T细胞,有效识别并杀死癌细胞。
但是,并非所有患者都能通过这些方法治疗,研究显示这些方法仅对少数癌症类型有效,并且CAR-T细胞疗法也有重大风险。
近期来自波士顿儿童医院发现了癌症免疫疗法的另外一种新武器,可以在更多的癌症类型中发挥作用。这种方法利用人体内免疫反应重新激活称为Gasdermin E的基因,这种基因在许多类型的癌症中均被抑制。
这一研究发现公布在3月11日的Nature杂志上。
该研究的主要研究者细胞和分子医学计划(PCMM)的Judy Lieberman医学博士说:“ Gasdermin E是一种非常有效的抑癌基因,但在大多数肿瘤组织中,它要么不表达,要么被突变,” “当激活肿瘤中的Gasdermin E时,它可以将免疫系统无法识别的具有免疫学意义的'冷'肿瘤转变为免疫系统可以控制的'热'肿瘤。”
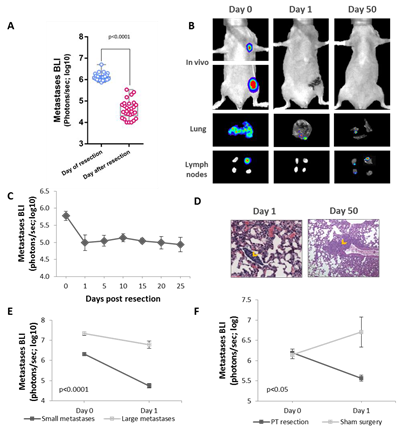
在这项研究中,Lieberman及其同事发现,他们测试的22种与癌症相关的突变中有20种导致降低了Gasdermin E的功能。当他们在小鼠模型中重新引入Gasdermin E时,发现能够触发pyroptosis,抑制多种肿瘤(三阴性乳腺癌,结肠直肠肿瘤和黑色素瘤)的生长。
加热免疫反应
研究小组还发现了在小鼠肿瘤细胞系中这个基因是如何发挥作用。通常,当包括大多数癌细胞的细胞死亡时,它是通过一种称为凋亡的过程,即安静,有序地死亡。但是,如果存在Gasdermin E并正常发挥作用时,癌细胞会通过一种高度炎性的细胞死亡形式(称为焦亡)死亡。
正如Lieberman的研究小组在活小鼠中显示的那样,这种发热听起来像是一种有效的免疫警报,可以募集杀伤性T细胞来抑制肿瘤。该团队目前正在研究诱导Gasdermin E增强抗肿瘤免疫反应的治疗策略。
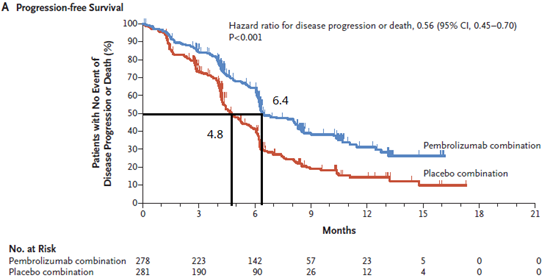
他说:“我们的建议是,如果能够打开炎症的危险信号,那么与其他免疫疗法相比,我们可以更充分地激活淋巴细胞,这具有更大的免疫力。将肿瘤中的炎症激活与检查点抑制剂药物相结合,可能比单独使用任何一种策略都更有效。”
原始出处:Zhang Z, Zhang Y, Xia S,et al. Gasdermin E suppresses tumour growth by activating anti-tumour immunity. Nature. 2020 Mar;579(7799):415-420.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗新方法#
46
#GAS#
47
#新发现#
45
#新方法#
39
#Nat#
40
#ASD#
34
为什么不检查下肢深静脉是否有血栓,如果朋友大量血栓介入科是否需要滤器治疗?这些问题都没交代!
102
这个可以
0