BJU Int:根治性前列腺切除术中阳性手术边缘分类的临床应用
2021-07-09 AlexYang MedSci原创
在根治性前列腺切除术(RP)样本中发现手术边缘阳性(PSM)意味着生化复发(BCR)的风险增加一倍。手术边缘状态包括两种,即阳性与阴性。在过去的十年中,人们越来越关注进一步的分类,包括PSM的数量、位
在根治性前列腺切除术(RP)样本中发现手术边缘阳性(PSM)意味着生化复发(BCR)的风险增加一倍。手术边缘状态包括两种,即阳性与阴性。在过去的十年中,人们越来越关注进一步的分类,包括PSM的数量、位置、长度和等级等参数都与BCR的预测有关。

近期,有研究人员确定了手术边缘阳性的分类是否能提高对生化复发的预测能力,并协助接受前列腺根治术的患者做出临床决策。
研究人员调查了2147名pT2和pT3a前列腺癌患者的详细手术边缘参数和生化复发状况。我们比较了一个基础模型,即从Memorial Sloan Kettering癌症中心术后列线图(前列腺特异性抗原、病理肿瘤分级和分期)中计算出的线性预测模型,并将手术边缘状态与5个其他的模型(基础模型加手术边缘亚分类)进行比较,以评估预测准确性的提高情况。另外,还进行了决策曲线分析来确定提高预测准确性参数的临床效用。
在2147名男性中,205人的手术边缘呈阳性,231人出现生化复发。加入手术边缘状态基础模型的区分度很高(c-index=0.801),但在全部队列中加入手术边缘亚分类则没有显著意义的改善。在仅考虑手术边缘阳性的男性的分析中(有生化复发的N=55),在基础模型中加入手术边缘亚分类,改善了对所有阳性边缘总长度的区分(分别为c-index改善=0.717至0.752和0.753)。决策曲线分析表明,增加这些参数后,对临床效用有一定的好处。
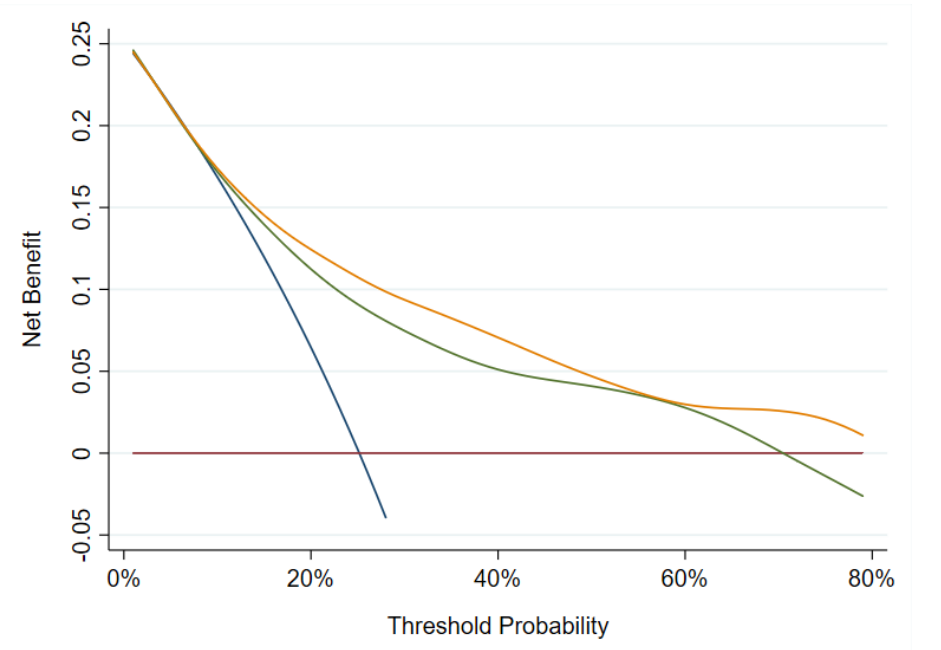
基础模型(绿色)与基础模型+阳性手术切缘总长度和切缘最大格林森等级模型(黄色)的净益处情况
综上所述,特定的亚分类参数增加了对生化复发的预测准确性,可能有助于手术边缘阳性患者的决策。这些发现可能对患者咨询和未来的辅助治疗试验设计有帮助。
原始出处:
Shawn Dason , Emily A Vertosick , Kazuma Udo et al. Clinical Utility of Subclassifying Positive Surgical Margins at Radical Prostatectomy. BJU Int. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
35
#临床应用#
44
#前列腺切除#
48
PSM
73
#根治#
34
有没有假阳性
70
学习了
54