Gastroenterology:肝硬化患者肠道微生物群也会发生明显改变
2020-10-16 MedSci原创 MedSci原创
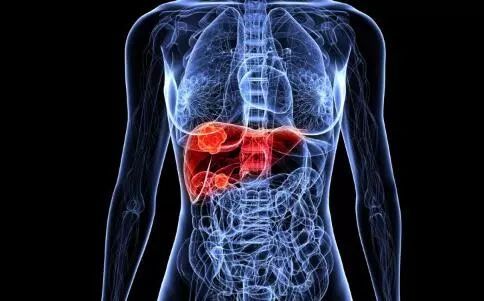
肝硬化与肠道微生物组组成的改变有关。尽管慢性肝衰竭急性发作(ACLF)是肝硬化最严重的临床阶段,但目前学界缺乏使用定量宏基因组学研究ACLF中肠道微生物组改变的研究。
背景与目标
肝硬化与肠道微生物组组成的改变有关。尽管慢性肝衰竭急性发作(ACLF)是肝硬化最严重的临床阶段,但目前学界缺乏使用定量宏基因组学研究ACLF中肠道微生物组改变的研究。因此,本项研究旨在对此进行相关探索。

方法
研究人员前瞻性收集了182例肝硬化患者的粪便样本。使用DNA文库的构建和测序对患者的粪便样本中的微生物组成进行测序。微生物基因被分组为簇,以宏基因组种(MGS)的方式进行展示。
结果
与健康受试者相比,肝硬化与基因和MGS丰富度的显着降低有关。这种丰富性的丧失与疾病阶段有关,此现象在ACLF患者中尤为明显,并在调整抗生素治疗后持续存在。ACLF与肠球菌显着增加有关。肠道微生物组改变与模型末期肝病(MELD)和Child-Pugh评分以及器官衰竭相关,以及尤其是肝性脑病和感染有关。有趣的是,肠道微生物组是3个月的生存期的有效预测因子,并具有良好的稳定性。
结论
肝硬化的特征是肠道微生物组发生明显改变,ACLF肝硬化阶段的改变最为明显。肠道微生物组的改变与肝硬化和生存的并发症有关。肠道微生物组可能导致疾病进展和不良预后。
原始出处:
Cristina Solé. Et al. ALTERATIONS IN GUT MICROBIOME IN CIRRHOSIS AS ASSESSED BY QUANTITATIVE METAGENOMICS. RELATIONSHIP WITH ACUTE-ON-CHRONIC LIVER FAILURE AND PROGNOSIS. Gastroenterology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Gastroenterol#
30
#微生物#
27
#GAS#
38
学习了正好需要
81
#AST#
28
肝硬化患者肠道菌群治疗的理论依据
90
#肠道微生物群#
43
#微生物群#
33
#Gastroenterology#
32
谢谢!最新的信息读起来就是收获大
40