World J Urol:继发于膀胱出口梗阻的持续或复发性下尿路症状的前列腺钬激光切除术的安全性和疗效分析
2021-06-25 AlexYang MedSci原创
前列腺钬激光剜除术(HoLEP)作为一种内窥镜替代方法已获得广泛接受,其安全性和有效性与经尿道前列腺切除术(TURP)相当。 此外,无论前列腺大小或抗凝状态如何,HoLEP都可以安全进行。最近,前列腺
前列腺钬激光剜除术(HoLEP)作为一种内窥镜替代方法已获得广泛接受,其安全性和有效性与经尿道前列腺切除术(TURP)相当。 此外,无论前列腺大小或抗凝状态如何,HoLEP都可以安全进行。最近,前列腺动脉栓塞(PAE)已成为前列腺增生症的另一种微创治疗选择。由于缺乏高水平的证据,目前美国泌尿外科协会(AUA)并不不推荐,但欧洲泌尿外科协会会推荐PAE给那些希望考虑微创治疗方案的男性。

近期,有研究人员评估了前列腺钬激光切除术(HoLEP)用于治疗先前前列腺动脉栓塞(PAE)后的持续或复发性下尿路症状的安全性和有效性,还评估了PAE后前列腺的组织病理学变化。
研究人员根据年龄、切除的前列腺组织的重量和抗凝状态,将10名事先进行PAE后接受HoLEP的患者与事先没有进行PAE的HoLEP患者按1:2的比例进行匹配,研究人员在匹配时对患者的结果未知。他们还对前列腺组织进行组织病理学检查,以寻找与先前PAE有关的变化。之后对患者的人口统计学、围手术期参数和随访数据进行了回顾性比较。
结果发现,PAE和HoLEP之间的中位时间间隔为25个月[IQR 14.5-37.5]。两组患者的人口统计学特征具有可比性。尽管之前有PAE,术中的切除平面保持良好。两组之间的手术时间、切除效率、血红蛋白下降、导尿时间和住院时间以及并发症的差异在统计学上不明显。两组中都有10%的样本发现了偶发的前列腺癌。PAE术后的前列腺标本显示了远处愈合的梗塞证据,表现为致密的透明少细胞结缔组织,周围有鳞状化生。另外,两组之间在AUA症状评分、最大尿流率、排尿后残余尿量以及3个月和6个月随访时的PSA方面没有统计学上的显著差异。
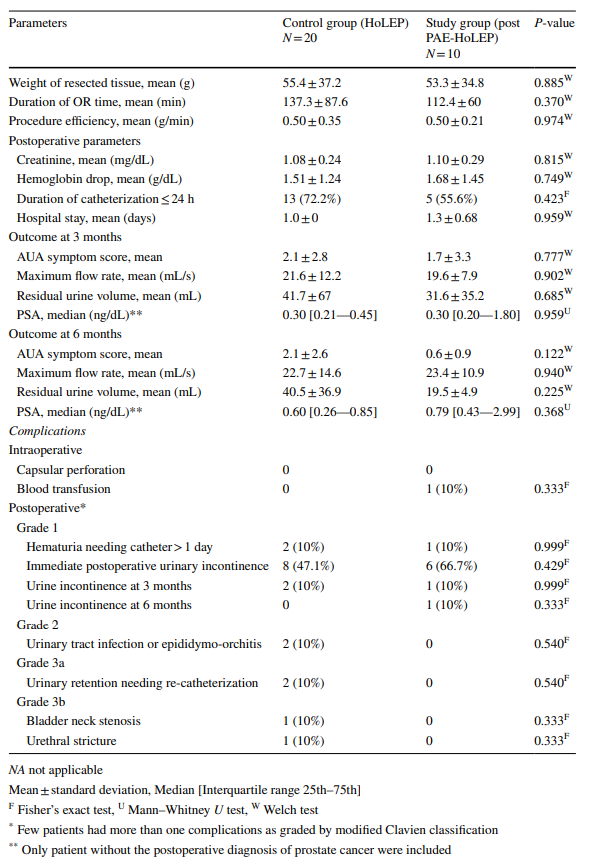
第6个月患者的术中和术后参数
综上所述,PAE后术中的切除平面保持良好。抢救性HoLEP在PAE后是安全和有效的,并能够产生与作为主要手术的HoLEP相当的结果。
原始出处:
Madhumita Parmar, Jonathan E Katz, Ruben Blachman-Braun et al. Safety and efficacy of holmium laser enucleation of prostate as salvage procedure for persistent or recurrent lower urinary tract symptoms secondary to bladder outlet obstruction after prior prostate artery embolization: a match analysis. World J Urol. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#复发性#
37
#疗效分析#
36
#尿路症状#
35
#继发#
34
#切除术#
41
#下尿路#
30
#激光#
36
#下尿路症状#
35
谢谢梅斯提供这么好的信息,学到很多
49