ACR:接受别嘌醇初始治疗的患者发生SCARs的风险升高
2013-04-09 ACR 丁香园
SCARs常发生于别嘌醇初始用药后的180天里 别嘌醇是一种黄嘌呤氧化酶抑制剂,具有抑制尿酸生成的作用。约2-5%的患者可能对别嘌醇存在过敏反应,表现为皮疹或胃肠道症状。与别嘌醇使用相关的皮肤副反应很罕见,但可能威胁生命。目前研究中,以人口学为基础,对这些药物反应的发生率及死亡率的研究报道较少。为明确这类严重副作用的发生率和死亡率,来自波士顿布利甘-妇女医院的SEOYOUNG C. KIM博士等
别嘌醇是一种黄嘌呤氧化酶抑制剂,具有抑制尿酸生成的作用。约2-5%的患者可能对别嘌醇存在过敏反应,表现为皮疹或胃肠道症状。与别嘌醇使用相关的皮肤副反应很罕见,但可能威胁生命。目前研究中,以人口学为基础,对这些药物反应的发生率及死亡率的研究报道较少。为明确这类严重副作用的发生率和死亡率,来自波士顿布利甘-妇女医院的SEOYOUNG C. KIM博士等研究者进行了一项队列研究。研究结果发表于2013年3月《关节炎治疗与研究》(Arthritis Care & Research)杂志上。研究认为,接受别嘌醇初始治疗的患者发生严重皮肤副反应(SCARs)的风险较高。
研究者采取匹配法对来自5个大型医疗补助项目的相关数据进行了分析,将初始使用别嘌醇的住院患者与那些未使用别嘌醇的患者数据进行对比,评估了各组患者SCARs的发生率(IR)和院内死亡率。主要结局通过诊断编码695.1来确定。使用Cox比例风险模型评估别嘌醇用药相关的SCARs风险,并确定别嘌醇剂量与SCARs风险的相关性。
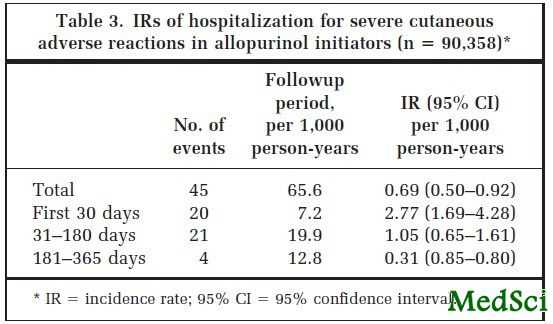
接受别嘌醇初始治疗的患者组中,在65625例患者-年的随访期里共出现了45例SCARs住院患者。每1000患者-年的粗IR为0.69(95%可信区间[95% CI] 0.50-0.92)。所有45例患者的药物反应均发生在别嘌醇初始治疗后的365天里,其中41例(91.1%)出现在用药后的180天里。12例患者(26.7%)在住院期间死亡。而未使用别嘌醇的患者组中,每1000患者-年的粗IR为0.04(95%CI 0.02-0.08)。别嘌醇初始治疗患者组较未使用别嘌醇患者组发生SCARs的风险增高(风险比[HR] 9.68,95%CI 4.55-20.57)。别嘌醇初始治疗组的患者经年龄、合并症及近期利尿剂用药史等因素调整后,高剂量别嘌醇组(>300mg/天)较低剂量别嘌醇组的HR为1.30(95%CI 0.31-5.36)。
研究者认为,在别嘌醇初始治疗的患者中,SCARs的发生率较低,但通常是致命性的,该反应常发生于初始用药后的180天里。别嘌醇初始治疗的患者较那些未使用别嘌醇的患者,其发生SCARs的风险增高了10倍。

Severe cutaneous reactions requiring hospitalization in allopurinol initiators: a population-based cohort study.
OBJECTIVE
Rare but potentially life-threatening cutaneous adverse reactions have been associated with allopurinol, but population-based data on the incidence and mortality of such reactions are scarce.
METHODS
We conducted a propensity score-matched cohort study to evaluate the incidence rate (IR) and in-hospital mortality of hospitalization for severe cutaneous adverse reactions (SCARs) in allopurinol initiators compared to non-allopurinol users, using data from 5 large Medicaid programs. The primary outcome was identified by the principal discharge diagnosis code 695.1. A Cox proportional hazards model evaluated the relative risk of SCARs associated with the use of allopurinol and determined the relative risk of SCARs associated with allopurinol dose.
RESULTS
During a followup period of 65,625 person-years for allopurinol initiators, 45 were hospitalized with SCARs. The crude IR was 0.69 (95% confidence interval [95% CI] 0.50-0.92) per 1,000 person-years. All 45 cases occurred within 365 days and 41 (91.1%) occurred within 180 days after initiating treatment with allopurinol. Twelve patients (26.7%) died during the hospitalization. The crude IR in non-allopurinol users was 0.04 (95% CI 0.02-0.08) per 1,000 person-years. The risk of SCARs was increased in allopurinol initiators versus nonusers (hazard ratio [HR] 9.68, 95% CI 4.55-20.57). Among allopurinol initiators, the HR for high-dosage (>300 mg/day) versus low-dosage allopurinol was 1.30 (95% CI 0.31-5.36) after adjusting for age, comorbidities, and recent diuretic use.
CONCLUSION
Among allopurinol initiators, SCARs were found to be rare but often fatal, and occurred mostly in the first 180 days of treatment. The risk of SCARs was 10 times as high in allopurinol initiators as compared to allopurinol nonusers.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#初始治疗#
33
#别嘌醇#
39
#ACR#
37