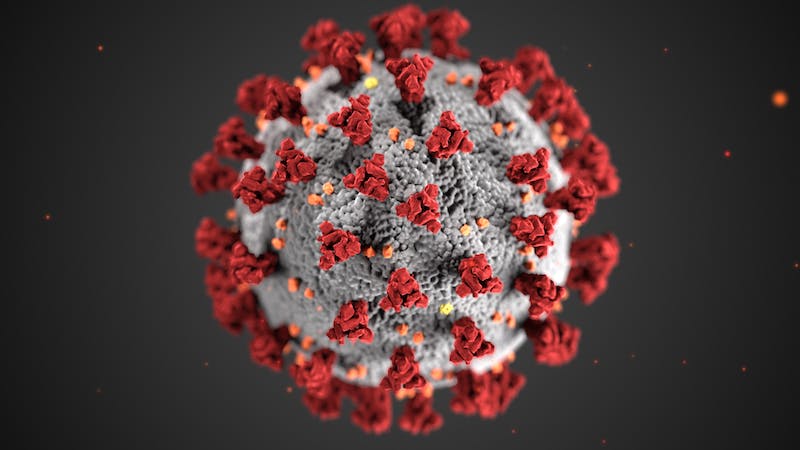
JAMA:皮质类固醇可提高COVID-19患者的生存率
2020-09-06 Allan MedSci原创
皮质类固醇(Corticosteroids)是由肾上腺皮质制造和分泌的类固醇激素,也可经由人工合成。它的药理作用复杂,且广泛涉及生理系统作用,如压力反应、免疫反应,以及发炎、糖类代谢作用、蛋白质分解代
皮质类固醇(Corticosteroids)是由肾上腺皮质制造和分泌的类固醇激素,也可经由人工合成。它的药理作用复杂,且广泛涉及生理系统作用,如压力反应、免疫反应,以及发炎、糖类代谢作用、蛋白质分解代谢、血液中电解质浓度等的控制。
现有证据表明,皮质类固醇可以显著改善重症COVID-19患者的预后,死亡风险可以降低多达20%。一项在JAMA上发表的研究(REMAP-CAP研究)表明,重症COVID-19患者接受氢化可的松治疗后有更好的康复机会。

REMAP-CAP和NIHR资助的RECOVERY试验获得的数据已经表明,类固醇地塞米松可以成功用于治疗中重度COVID-19,皮质类固醇可以最大程度地降低死亡风险(高达20%)。这些发现提供了进一步的证据,表明糖皮质激素可能是重症患者COVID-19治疗的重要组成部分。虽然类固醇不是治愈方法,但它们有助于改善治疗结局。
原始出处:
http://www.pharmatimes.com/news/corticosteroids_boost_survival_rates_for_covid-19_patients_1348215
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#生存率#
35
#COVID-19患者#
27
#类固醇#
31
emmm…如果能见要说下为什么就好了…
101
棒
92
学习
96
机制是什么呢
90
学习
83
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
23
下载,好文章
29