度伐利尤单抗治疗局部晚期宫颈癌III期研究,结果失败
2022-04-02 网络 网络
3月24日,阿斯利康宣布,PD-L1单抗Imfinzi (度伐利尤单抗) 联合放化疗(CRT)治疗局部晚期宫颈癌的III期CALLA研究未达到改善无进展生存期(PFS)的主要终点。与单纯放化疗相比,P
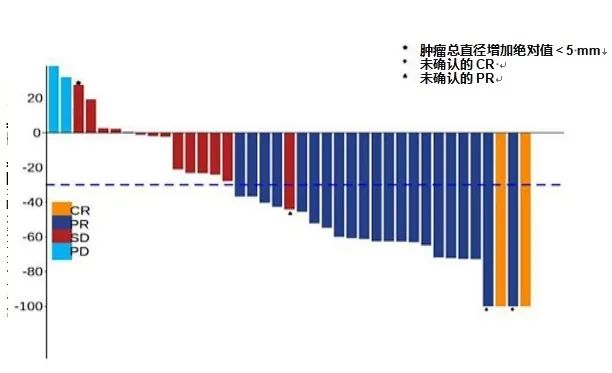
3月24日,阿斯利康宣布,PD-L1单抗Imfinzi (度伐利尤单抗) 联合放化疗(CRT)治疗局部晚期宫颈癌的III期CALLA研究未达到改善无进展生存期(PFS)的主要终点。与单纯放化疗相比,PFS未实现统计学意义改善。
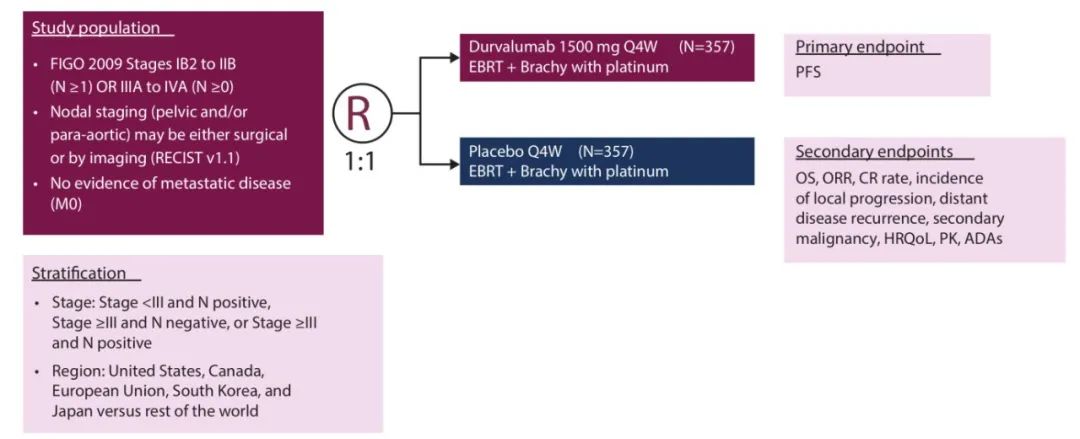
CALLA研究是一项随机、多中心、双盲、全球性III期临床试验,最终770名局部晚期宫颈癌患者接受了标准治疗CRT联合1500 mg固定剂量Imfinzi或安慰剂治疗,受试者每四周治疗一次,持续24个周期或直到疾病进展。该试验在包括美国、欧洲、拉丁美洲、非洲和亚洲在内的15个国家的120个中心进行。主要终点为无进展生存期(PFS),主要次要终点包括总生存期、安全性和耐受性。
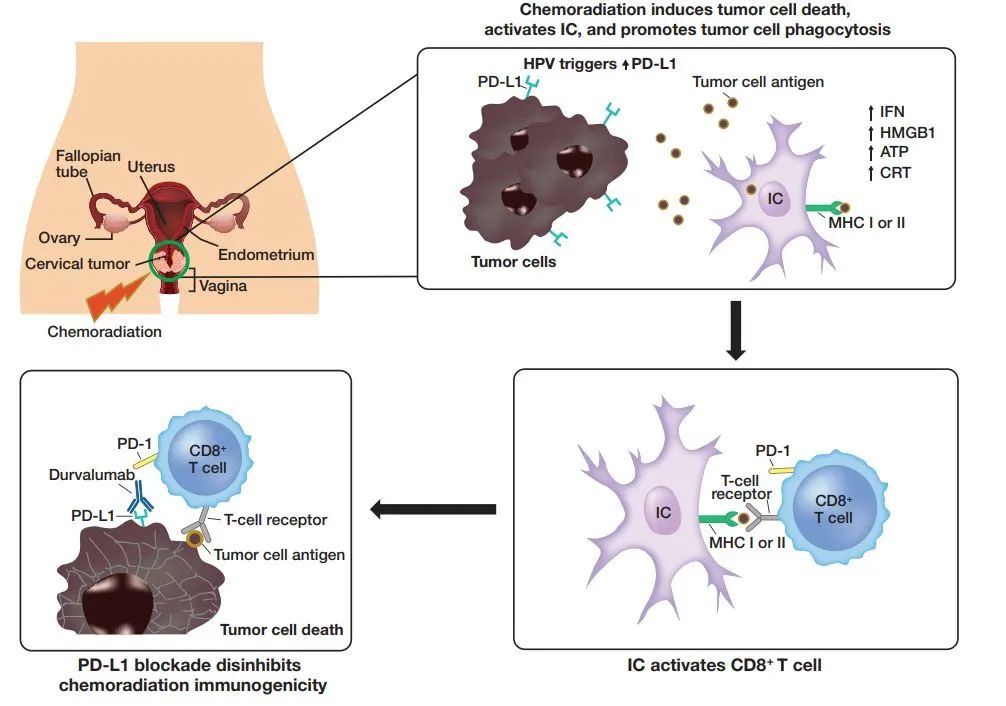
宫颈癌是全球第八大最常见、第九大最致命的癌症,每年约有60万确诊病例。约40-50%宫颈癌患者确诊时已处于局部晚期。按照目前的治疗标准铂类化疗联合放疗,局部晚期宫颈癌患者的复发率约为40%,5年生存率约为65-70%。临床前数据显示,同步放化疗联合阻断PD-1/L1途径可通过启动DNA断裂、细胞死亡、吞噬作用和抗原呈递来诱导免疫原性环境增加,从而导致免疫介导的肿瘤重新激活和增强的抗肿瘤活性。
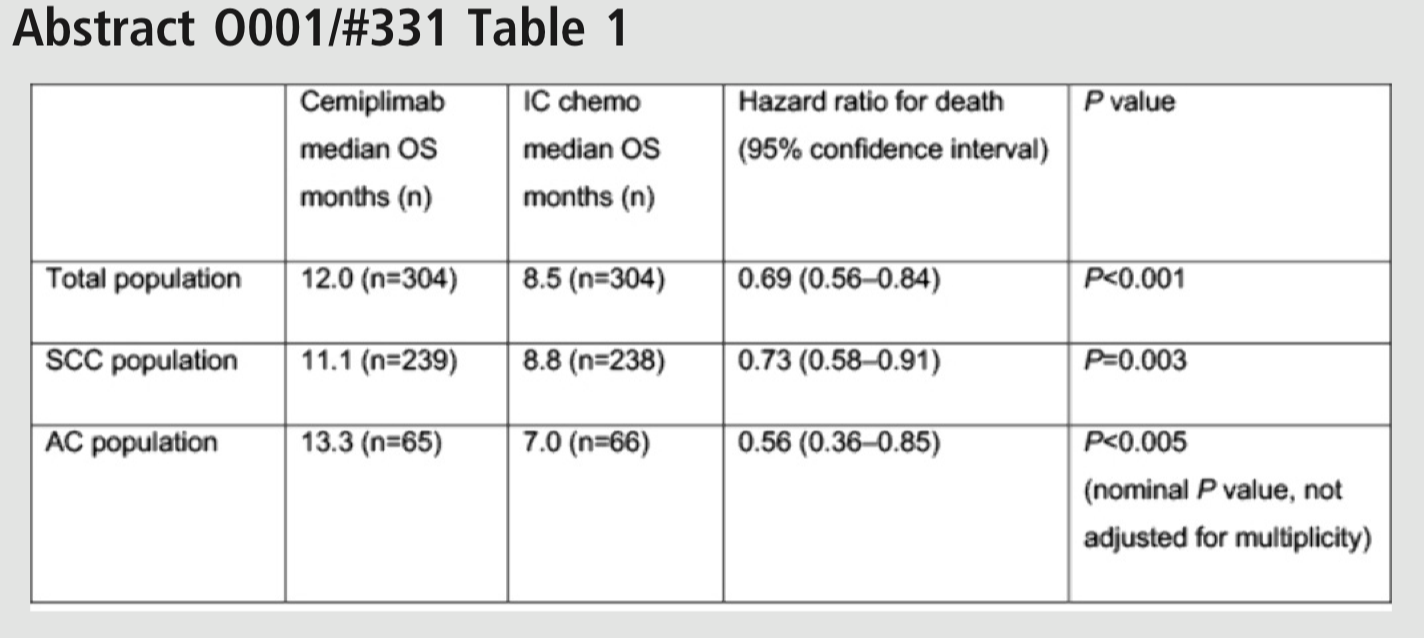
在这一领域,阿斯利康对Imfinizi寄予厚望,希望可以与默沙东的 PD-1帕博利珠单抗展开竞争。帕博利珠单抗在2021年10月获得了与化疗联合治疗持续性、复发性或转移性宫颈癌的一线疗法资格。CALLA研究的失败使得阿斯利康希望破灭,但这并不是PD-1/L1疗法的首次失利。2022年1月,作为首个在III期临床中证明可改善铂类化疗后疾病进展总生存期的PD-L1抗体西米普利单抗也撤销了该适应症;再往前述,PD-1抗体巴替利单抗也在2021年撤销了宫颈癌的上市申请。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#III#
42
#III期研究#
38
#局部晚期#
37
#局部#
40
#宫颈#
45
#III期#
47
#晚期宫颈癌#
45
#学习#可惜了
46