IMpower010研究生存数据首次公布,夯实阿替利珠单抗为标准辅助治疗方案!| WCLC 2022速递
2022-08-13 MedSci原创 MedSci原创
WCLC:III 期研究IMpower010:阿替利珠单抗对比最佳支持治疗在可切除非小细胞肺癌(NSCLC)患者中的中期总生存期(OS)结果
IMpower010 (NCT02486718)的既往数据表明,在铂类化疗后切除的NSCLC患者中,阿替利珠单抗与最佳支持治疗(BSC)相比,无病生存(DFS)有统计学显著获益:PD-L1肿瘤细胞(TC)≥1% II-IIIA患者(DFS HR=0.66),II-IIIA患者(DFS HR=0.79)。基于这些发现,在美国、中国和其他国家,阿替利珠单抗被批准作为程序死亡配体1 (PD-L1)肿瘤细胞(TC)≥1% II-IIIA期NSCLC患者切除和铂基化疗后的辅助治疗。在IMpower010 DFS中期分析(IA)中,关键的次级OS终点还不成熟,但已在这一治疗环境中具有相当的临床意义。本次WCLC大会上公布了额外随访13个月的研究结果。
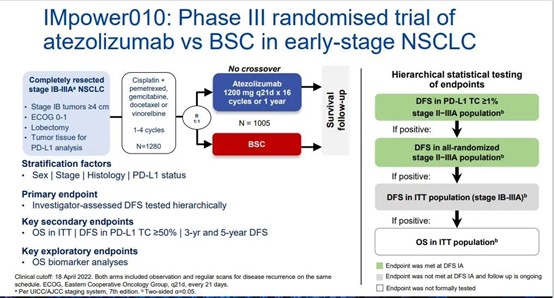
符合条件的患者完全切除了IB期(肿瘤≥4cm)-IIIA NSCLC (AJCC/UICC v7),且ECOG PS 0-1。患者接受1-4个21天周期的顺铂双联化疗(入组期),随后按1:1随机分组,接受16个周期的阿替利珠单抗1200 mg q3w或BSC辅助治疗(随机期)。主要终点为分层试验DFS;关键次要终点包括OS (ITT人群)和安全结果。此分析首次公布预设OS中期分析结果;如果ITT人群的DFS在最终DFS分析时达到统计显著性,将正式测试该人群的OS。
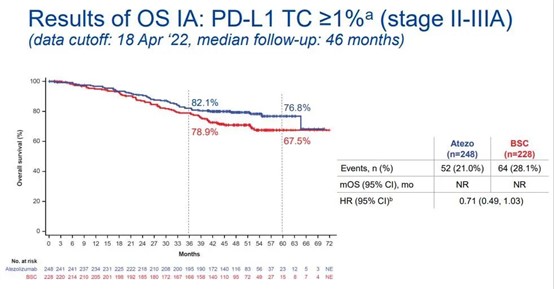
在临床截止日期(2022年4月18日),中位随访时间为45个月,25.0%的患者死亡(ITT人群;N = 1005)。在PD-L1 TC≥1%的II-IIIA期患者中,观察到阿替利珠单抗组的OS获益倾向(OS HR=0.71)。

阿替利珠单抗组和BSC组患者中分别有22.0%和11.5%患者发生3-4级不良事件(AE),两组的5级AE发生率为分别为 0.8%和0%。在接受阿替利珠单抗治疗的患者中,52.1%发生特殊的AE;7.9%为3-4级,0.4%为5级(肺炎/间质性肺疾病和心肌炎)。DFS IA临床截止日期后未发生新的5级AE。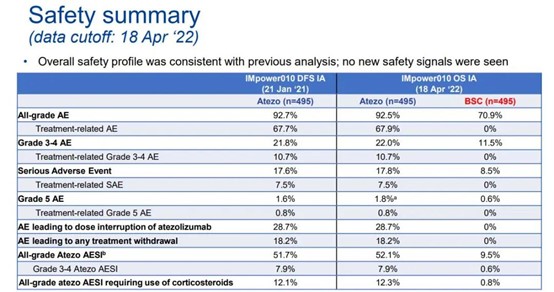
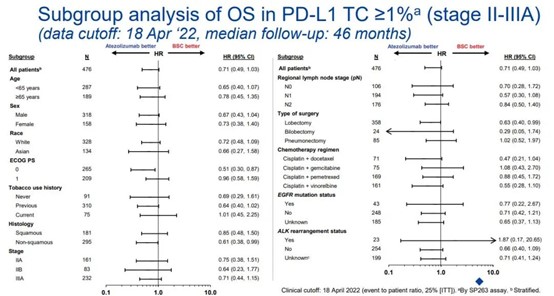
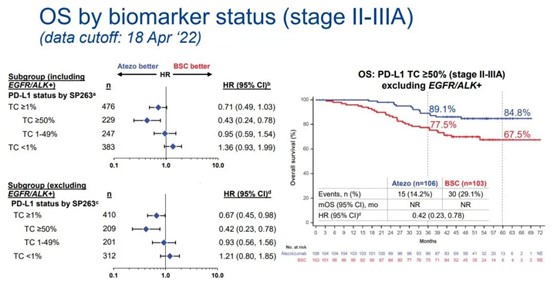
结果表明,在首次OS中期分析时,在PD-L1 TC≥1%的II-IIIA期患者中观察到阿替利珠单抗组的OS获益倾向,在PD-L1 TC≥50% II-IIIA期患者中,阿替利珠单抗辅助治疗显示有临床意义的OS获益(HR=0.43)。但在完全随机化的II-IIIA期或ITT人群中未观察到这种获益区属。在后续随访中未观察到新的安全信号。IMpower010将继续进行最终的DFS分析,并提供进一步的OS结果。
本次公布的IMpower010研究OS中期分析数据,成功地证明了DFS获益转化为远期的OS获益,进一步证实阿替利珠单抗辅助治疗是目前新的辅助治疗标准方案。对于PD-L1 TC≥1%的II-IIIA期患者应进行阿替利珠单抗辅助免疫治疗,尤其是对PD-L1 TC≥50%的患者。这会使早期可手术NSCLC患者的生存率再创新高,远超过单纯手术和手术+辅助化疗的水平,真正让患者有治愈的可能性。
原文来源:
PL03.09 - IMpower010:Overall Survival Interim Analysis of a Phase III Study of Atezolizumab vs Best Supportive Care in Resected NSCLC.2022 WCLC.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#生存数据#
57
#研究生#
54
#替利珠单抗#
60
#治疗方案#
81
#power#
50
#WCLC#
41
#MPO#
40