JE:左金丸减轻幽门螺杆菌诱导的慢性萎缩性胃炎
2021-11-26 Vivi MedSci原创
左金丸通过JMJD2B/COX-2/VEGF轴和HMGB1/NF -κB信号通路抑制幽门螺杆菌诱导的炎症反应,从而防止胃粘膜损伤,改善慢性萎缩性胃炎。
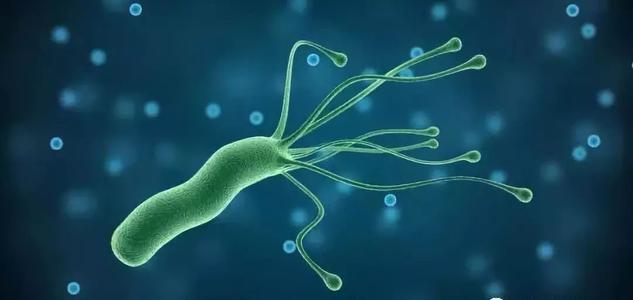
研究背景:慢性萎缩性胃炎(CAG)是一种常见的消化系统疾病,幽门螺杆菌感染可诱发CAG,最终可导致胃癌。左金丸出自《丹溪心法》,由黄连、吴茱萸按6:1组成,具有泻肝火,行湿,开痞结之功效,主治肝火犯胃,嘈杂吞酸,呕吐胁痛,筋疝痞结,霍乱转筋。左金丸被列入《中国药典》(2015年版),是临床上治疗食管炎、胃炎、消化性溃疡等疾病的常用方剂。左金丸已广泛应用于临床,其治疗CAG的机制尚不清楚。

研究方法:建立幽门螺杆菌诱导SD大鼠CAG模型(对照组,模型组,左金丸低、中、高剂量组,奥美拉唑组),通过胃组织病理学和血清炎症因子检测大鼠的炎症水平和黏膜损伤。通过GES-1细胞模型检测左金对细胞活力和形态的改善。此外,通过检测JMJD2B/COX-2/VEGF轴和HMGB1/NF-κB信号通路的相对mRNA和蛋白表达水平,进一步了解左金丸对幽门螺杆菌诱导CAG的治疗作用和可能的机制。
研究结果:模型组血清IL-6、MCP-1、PGE2、TNF-α、VEGF水平较对照组显著升高。与模型组相比,左金丸高剂量组(2.52 g / kg)可显著降低血清IL-6、MCP-1、PGE2、TNF-α、VEGF水平。
病理学观察显示,对照组大鼠粘膜完整,有紧密、丰富、有序的胃腺。CAG模型大鼠固有腺体缺失,黏膜部分脱落,黏膜中性粒细胞浸润。奥美拉唑组和左金丸组大鼠水肿、充血、糜烂、萎缩明显改善。其中,高剂量组炎症细胞浸润显著减少,胃粘膜损伤减少。结果表明,不同浓度的左金丸对黏膜腺体有不同程度的修复作用,表明左金丸对幽门螺杆菌诱导的CAG大鼠有一定的治疗作用。
CCK-8法检测GES-1细胞活力结果表明,60 μg/mL左金丸对细胞有较好的保护作用,以其为最佳浓度考察其保护作用。此外,较低MOIs(10:1, 20:1, 50:1)的幽门螺杆菌感染导致JMJD2B剂量依赖性表达,最终选择MOI 50:1持续12 h的感染进行进一步研究。荧光染色成像结果表明,左金丸能促进GES-1细胞增殖,改善幽门螺杆菌诱导的胃上皮细胞损伤。
大鼠免疫组化结果显示,模型组的JMJD2B、COX-2表达水平高于对照组,左金丸治疗降低了JMJD2B、COX-2的表达量。体内外RT-qPCR和western blotting结果显示,与对照组相比,幽门螺杆菌感染能显著提高JMJD2B、COX-2、VEGF、VEGFR1和VEGFR2 蛋白和mRNA相对表达量。左金丸治疗可显著降低这些mRNA和蛋白的表达,且高剂量组的效果更显著。
此外,幽门螺杆菌能显著提高大鼠和GES-1细胞中HMGB1、MyD88和RAGE mRNA相对表达量。左金丸处理降低了这些基因的表达水平,其中高剂量组最显著。与对照组相比,感染幽门螺杆菌后HMGB1、NF-κB p65和RAS蛋白表达显著增加,左金丸可剂量依赖性地降低HMGB1、NF-κB p65和RAS蛋白表达。免疫荧光显示,感染幽门螺杆菌导致HMGB1表达升高和NF -κB p65核易位,这一趋势是通过左金丸治疗改善。这些结果表明左金丸可以通过降低HMGB1 / NF -κB信号通路表达改善幽门螺杆菌感染导致的胃损伤和炎症。
研究结论:左金丸通过JMJD2B/COX-2/VEGF轴和HMGB1/NF -κB信号通路抑制幽门螺杆菌诱导的炎症反应,从而防止胃粘膜损伤。该研究结果提示左金丸在CAG治疗中的潜在作用,有待进一步研究。
文献来源:
Wen J, Wu S, Ma X, Zhao Y. Zuojin Pill attenuates Helicobacter pylori-induced chronic atrophic gastritis in rats and improves gastric epithelial cells function in GES-1 cells [published online ahead of print, 2021 Nov 19]. J Ethnopharmacol. 2021;114855. doi:10.1016/j.jep.2021.114855
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#萎缩#
35
#萎缩性#
36
#螺杆菌#
52
学习
54
学习
48
学习
62
学习了
61
学习了
58
学习了
43
学习
30