Aging Cell:维生素D受体激活可能会增加阿尔茨海默病风险
2021-11-03 haibei MedSci原创
VDR水平的异常增加被发现与Aβ斑块、胶质增生和自噬体共同定位,暗示VDR在AD发病机制中的非基因组激活。
随着世界人口的老龄化,痴呆症的发病率越来越高。阿尔茨海默病(AD)占所有痴呆症病例的60%-80%,但目前还没有发现可以预防或减慢这种疾病进展的疗法。许多流行病学研究表明,维生素D的缺乏与AD和其他痴呆症有关。然而,与维生素D相关的AD的发病机制仍不清楚。维生素D除了对矿物质和骨骼平衡有众所周知的贡献外,还对发育中的大脑产生神经营养或神经保护作用。
然而,维生素D不是一种维生素,而是一种类固醇激素。像其他类固醇激素一样,维生素D可能引发基因组和非基因组的细胞反应。维生素D的基因组作用是通过与维生素D受体(VDR)结合启动的。更具体地说,维生素D的代谢物1α,25-二羟基维生素D3(或钙三醇)可以与VDR结合。与配体结合的VDR更倾向于与视黄醇X受体(RXR)二聚,以对靶标基因进行转录调节,例如,CYP24A1,一种关键的维生素D分解酶。
目前,已经有很多证据表明维生素D在大脑中发挥基因组作用,VDR已被发现在介导大脑发育和功能的主要脑细胞类型中广泛表达。

同时,维生素D也在大脑中发挥非基因组作用。VDR的非基因组作用是对细胞刺激的快速质膜反应,但似乎不需要VDR-RXR相互作用。VDR还参与异物代谢,与维生素D结合无关。众所周知,可溶性毒性Aβ原纤维会导致AD的神经变性。然而,非基因组的VDR途径是否在AD中发挥作用仍不清楚。到目前为止,大多数研究都集中在调查VDR的遗传变异与AD风险的关系。有一些常见的VDR基因多态性与AD的发病率有关。
最近,研究人员利用死后的人脑、APP/PS1小鼠和细胞培养物调查了VDR在AD中的作用。耐人寻味的是,尽管维生素D在AD患者和小鼠中减少,但海马VDR水平却反过来增加。VDR水平的异常增加被发现与Aβ斑块、胶质增生和自噬体共同定位,暗示VDR在AD发病机制中的非基因组激活。
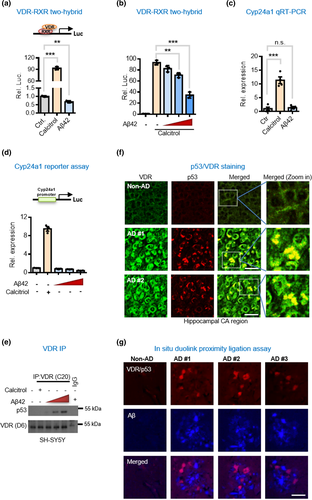
Aβ42破坏了基因组的VDR/RXR复合物,并诱导形成VDR/p53非基因组复合物。
此外,机制研究显示,Aβ在没有其典型配体维生素D的情况下上调了VDR,并将其异构体结合伙伴从RXR换成了p53。VDR/p53复合物主要定位在细胞膜上,增加了神经元自噬和凋亡。通过化学方法抑制p53, 使VDR转回RXR,逆转了AD小鼠的淀粉样变和认知障碍。
这些结果表明,VDR与p53的非基因组重合是AD进展的关键,因此VDR/p53途径可能是治疗AD患者的目标。
原始出处:
Rai-Hua Lai et al. Non-genomic rewiring of vitamin D receptor to p53 as a key to Alzheimer's disease. Aging Cell (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Cell#
46
#阿尔茨#
55
#CEL#
52
#阿尔茨海#
55
#阿尔茨海默#
51