Cardiovasc Diabetol:达格列净、艾塞那肽及其联合应用于2型糖尿病患者降压作用的机制
2022-05-03 从医路漫漫 MedSci原创
血压(BP)的降低可能在一定程度上有助于改善心血管结局。SLGT2i的降压作用约为4mm Hg。

背景:2型糖尿病(T2D)与心血管疾病(CV)的发病率和死亡率有关,这是由于高血糖和频繁相关的肥胖、血脂异常和高血压的共同作用。在过去的几十年里,已经开发了两类新的药物来降低多种心血管危险因素:钠-葡萄糖共转运体2的抑制剂(SGLT2i)和胰高血糖素样肽-1受体激动剂(GLP-1RAs)。SGLT2i可改善心血管预后(3-MACE),特别是心力衰竭(住院),并改善动脉粥样硬化性疾病患者的死亡率,无论是否存在糖尿病,这表明心血管益处不仅仅是降糖。血压(BP)的降低可能在一定程度上有助于改善心血管结局。SLGT2i的降压作用约为4mm Hg。血压降低效应的潜在机制仍不完全清楚,但持续减少的血浆容量可能起到作用。由于血浆容量和(动脉)血压的减少不会增加心率(HR),因此有人认为交感神经系统(SNS)的活动也会减少。动脉僵硬的改善和内皮功能的改善也被认为有助于长期降低血压。
与SGLT2i类似,GLP-1RAs可降低T2D患者的心血管疾病(CVD),其作用模式也不完全清楚,但可能是多因素的。GLP-1RAs降低血压(降低的大小取决于所使用的药物),这可能有助于降低心血管疾病。GLP-1-RA降压作用的机制可能包括降低血管阻力、排钠和减轻体重。
目的:本研究的目的是评估SGLT2i达格列净、GLP-1RA埃塞那肽和达格列净-埃塞那肽与安慰剂相比在肥胖症和2型糖尿病患者中降低血压的机制。
方法:66例2型糖尿病患者随机分为达格列净10 mg/d、埃塞那肽10µg/d、达格列净-埃塞那肽或安慰剂治疗16周。在治疗10天和16周后,评估治疗对以下指标的影响:(1)血浆容量(按Strauss公式计算)、生物阻抗谱、红细胞压积、(2)自主神经系统活动(心率变异性)、(3)动脉僵硬(脉搏波压平法)、(4)全身血流动力学参数(包括外周血管阻力、心输出量和每搏量)(均来自非侵入性全身血流动力学监测),(5)钠尿(24小时尿收集)。
结果:用药10d后,达格列净使血压下降4.7 mm Hg,收缩压下降,血浆容量减少。16周后,达格列净使血压下降4.4毫米汞柱,并降低交感神经系统活动。治疗10天和16周后,艾塞那肽对SBP无影响,但降低副交感神经系统活动。治疗10天后,达格列净-埃塞那肽使血压下降4.2 mm Hg,血浆量减少。治疗16周后,达格列净-埃塞那肽使血压下降6.8 mm Hg,血浆容量仍有下降,但对SNS值无明显影响。
表1 血压和心率的变化

表2心血管功能指标

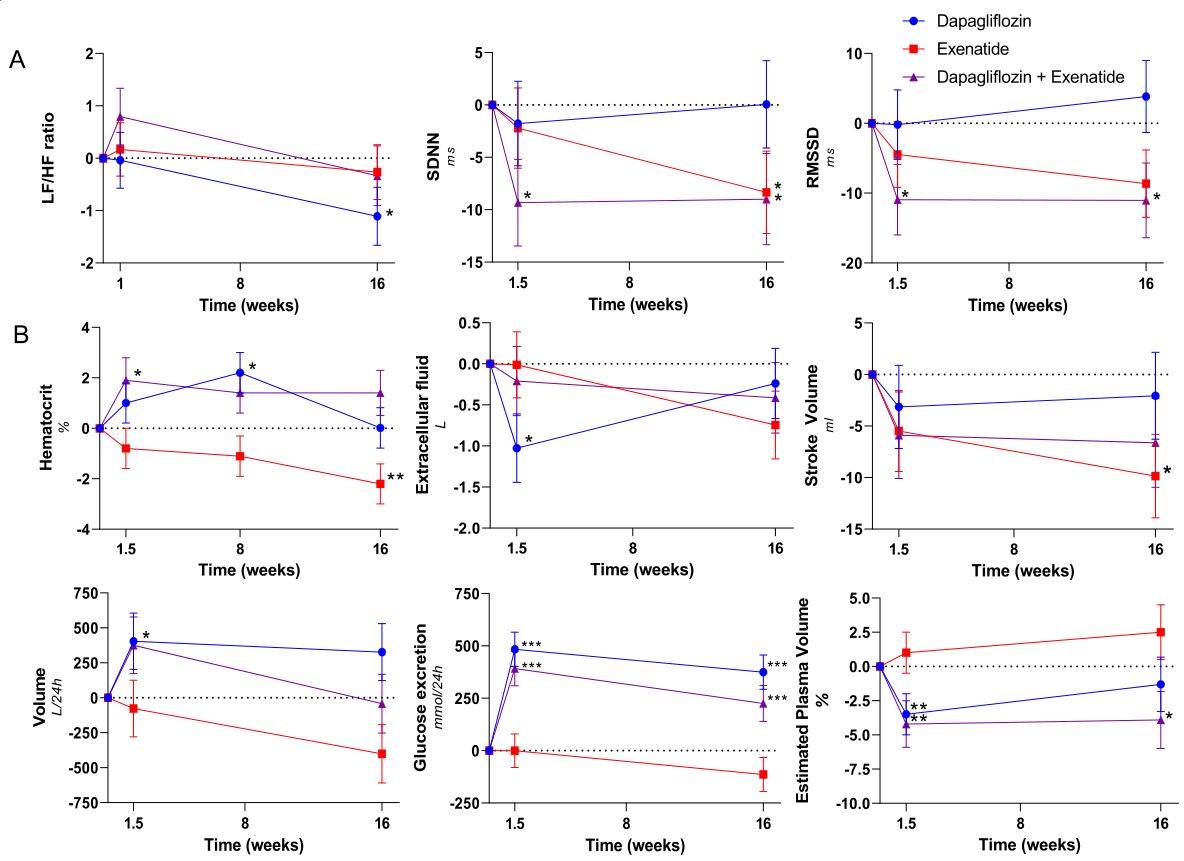
图1线性混合模型用于比较基线校正治疗和安慰剂的效果。达帕利嗪(蓝圈)、艾塞那肽(红方)、达帕利嗪加艾塞那肽(紫色上三角)治疗10天、16周后,A、B自主神经平衡的变化。数据点用扫描电子显微镜表示平均值。经基线值校正后,治疗组与安慰剂组比较,差异有统计学意义:*(P<0.001)、**(P<0.01)、*(P<0.05)。
结论:达格列净引起的血浆容量收缩可能参与了SBP的初始下降,而SNS活性的降低可能是持续SBP下降的原因之一。达格列净-埃塞那肽的SBP降幅最大。对血浆容量的影响与达格列净单药相当,SNS活性没有降低,因此可能有其他机制有助于该联合用药的降压作用,有待进一步研究。
原文出处:van Ruiten CC, Smits MM, Kok MD, et al.Mechanisms underlying the blood pressure lowering effects of dapagliflozin, exenatide, and their combination in people with type 2 diabetes: a secondary analysis of a randomized trial.Cardiovasc Diabetol 2022 Apr 28;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
38
#联合应用#
42
#DIA#
44
#BET#
44
#降压#
42
#2型糖尿病患者#
32
#艾塞那肽#
51
#糖尿病患者#
34
学到了
57