Acta Oncol:在临床试验之外接受治疗的慢性期老年慢性粒细胞白血病患者中一线达沙替尼的长期随访: 一项现实生活中的队列观察研究
2022-01-25 MedSci原创 MedSci原创
DAS 可能对受 CP-CML 影响的老年患者(年龄>75 岁)有效,且毒性可接受。
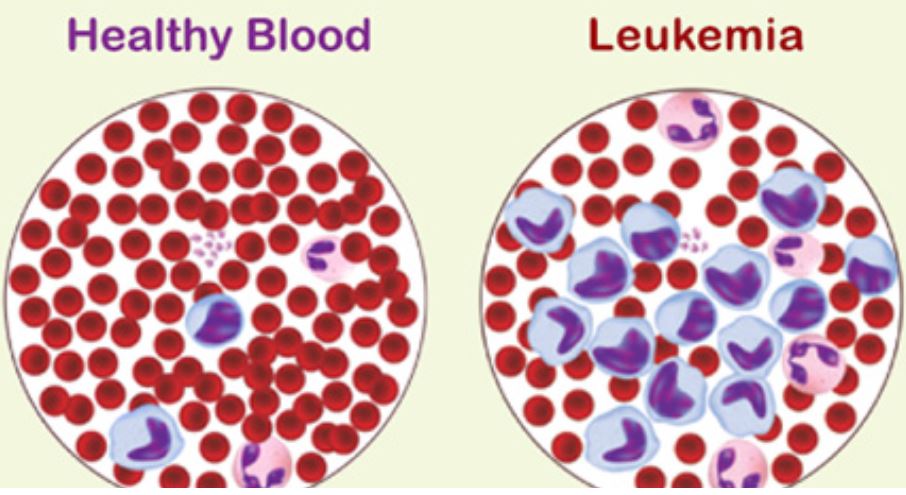
自酪氨酸激酶抑制剂(TKIs)的引入以来,慢性髓系白血病(CML)的临床情况已经发生了显著的变化。在大多数情况下,需要长期治疗和分子监测,预期寿命接近一般人群,并允许在大量患者中实现深度分子反应(DMR)。第二代TKIs尼洛替尼(NIL)和达沙替尼(DAS)首次作为im耐药或不耐受的CML患者的二线药物引入,然后被批准为一线治疗。尽管有这些突出的结果,在一线接受第二代酪氨酸激酶抑制剂治疗的年龄 >75 岁的慢性期慢性粒细胞白血病 (CP-CML) 患者中的数据数量有限。
因此,为了解决达沙替尼 (DAS)治疗的这个问题,研究人员回顾性分析了 45 名 CP-CML 患者 (pts),他们在 20 个意大利中心进行了随访,并在一线接受了达沙替尼 (DAS) 治疗。
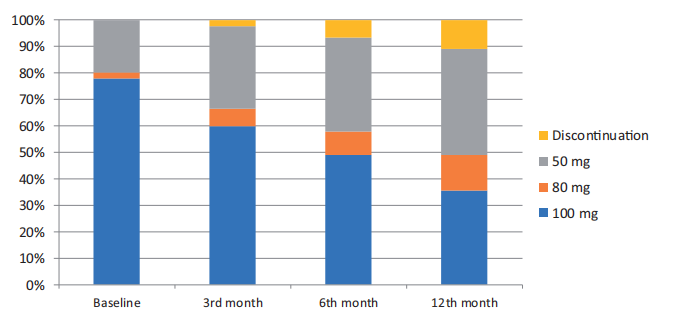
图1:不同治疗时间点的达沙替尼剂量。
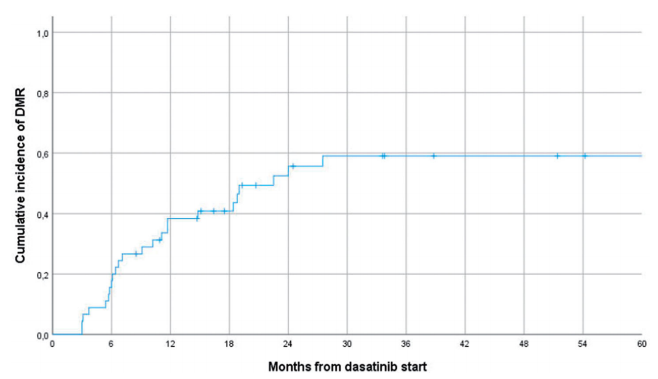
图2:深层分子反应的累积发生率。
患者中位年龄为 78.4 岁(范围 75-89.2 岁)。DAS 起始剂量分别为 100 mg QD 35 例 (77.7%)、80 mg QD 1 例 (2.2%) 和 50 mg QD 9 例 (20.1%)。中位随访时间为 42.6 个月(IQR 20.4 - 63.3)。

图3:无事件生存。
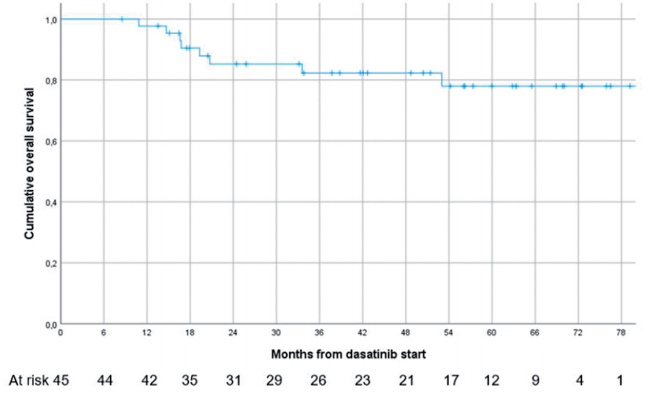
图4:总生存率。
结果提示,分别在 6 例(13.3%)和 12 例(26.6%)患者中检测到 3 级和 4 级血液学和非血液学副作用。在中位 DAS 暴露期 14.7 个月 (IQR 3.0 - 33.1) 后,有 13 名患者 (28.8%) 发生了所有级别的胸腔积液。DAS 剂量减少和永久停药率分别为 53.3% 和 20.0%。作为最佳反应,42/45 (93.3%) 的患者达到完全细胞遗传学反应 (CCyR),35/45 (77.7%) 的主要分子反应 (MMR) 和 24/45 (53.3%) 的深度分子反应(均MR 4.0 和 MR 4.5)。只有 1 名患者(2.2%)在治疗 13 个月后进入急变期;观察到 8 例死亡(1 例与 CML 相关,7 例与 CML 无关)。36 个月时的累积无事件生存率和总生存率分别为 64.7%(95%,CI 49.4 - 80.0)和 82.3%(95%,CI 70.3-94.3)。
总的来说,这些发现虽然在有限和选定的患者队列中进行了评估,但表明 DAS 可能对受 CP-CML 影响的老年患者(年龄>75 岁)有效,且毒性可接受。
原始出处:
Stagno F, Breccia M, Annunziata M, Trawinska MM, Iurlo A, Sgherza N, Fava C, Gozzini A, Luciano L, Carmosino I, Bonifacio M, Sorà F, Leonetti Crescenzi S, Crugnola M, Gugliotta G, Galimberti S, Bucelli C, Colafigli G, Feo C, Tiribelli M, Mauro E, Russo Rossi A, Guarini A, Abruzzese E, Rosti G, Di Raimondo F, Latagliata R. Long term follow-up of frontline Dasatinib in older patients with chronic myeloid leukemia in chronic phase treated outside clinical trials: a real-life cohort observational study. Acta Oncol. 2021 Nov;60(11):1527-1533. doi: 10.1080/0284186X.2021.1971292. Epub 2021 Sep 9. PMID: 34499575.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Oncol#
25
#CTA#
28
#观察研究#
46
#长期随访#
53
#达沙替尼#
45