肺原发黑色素瘤一例
2020-08-07 卞巍,张敏鸣 临床放射学杂志
患者女,65岁。无明显诱因出现咳嗽2周,以连续性干咳为主,无咳痰,未诉发热,有头晕头痛、胸闷气促、夜间盗汗,当地医院查胸部CT示:右下肺占位性病变。治疗后上述症状有好转(具体用药不详),为进一步治疗来
患者女,65岁。无明显诱因出现咳嗽2周,以连续性干咳为主,无咳痰,未诉发热,有头晕头痛、胸闷气促、夜间盗汗,当地医院查胸部CT示:右下肺占位性病变。治疗后上述症状有好转(具体用药不详),为进一步治疗来浙江大学附属第二医院检查。
体检:皮肤、黏膜无特殊,浅表淋巴结未触及。妇科会诊提示外阴无特殊,阴道壁未见明显肿块或色素沉着,宫腔光滑。腹部及浅表淋巴结B超均未见阳性发现。头颅CT增强扫描未见明显占位。
胸部CT平扫加增强扫描示(图1、2):右肺下叶肿块,边界清晰,大小约2.9 cm×2.1 cm,CT值约45HU,增强后呈持续强化,且强化欠均匀,CT值约105HU。诊断:肺良性病变可能性大,必要时穿刺活检。胸部MRI平扫加增强扫描示(图3~5):右肺下叶后基底段见一异常结节信号,大小约2.5 cm×1.9 cm×2.5 cm,边界较清,T2WI呈高信号,内见条片状低信号,抑脂T1WI为高信号,内见斑片状低信号,扩散加权成像(DWI)序列示肿块内见结节状扩散受限区。增强后病灶强化不明显。诊断:右肺下叶后基底段结节,考虑黑色素瘤。
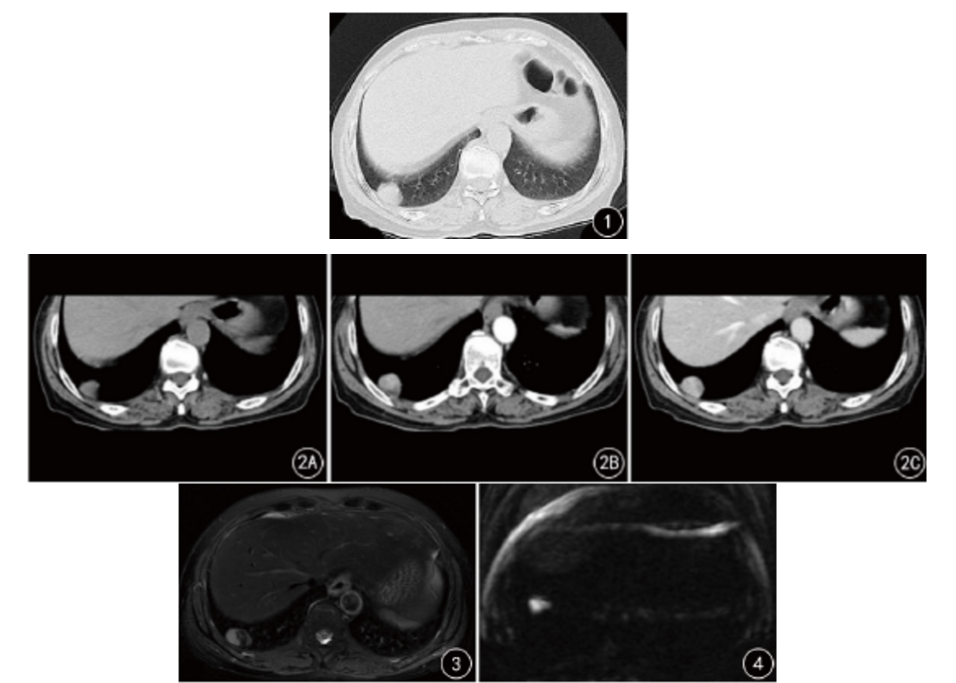
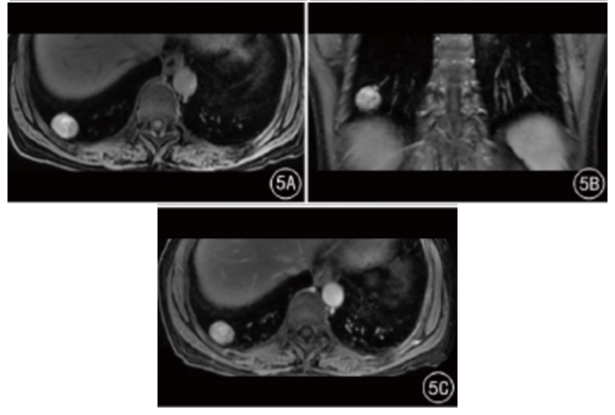
图1CT平扫肺窗:右肺下叶高密度肿块,边界清晰;图2A~CCT纵隔窗:肿块增强扫描前后对比,呈明显持续强化;图3MRI平扫:T2WI肿块内部低信号;图4DWI示:肿块扩散受限;图5A~C MRI增强扫描前后抑脂T1WI:增强扫描前肿块为高信号,内见斑片状低信号,增强扫描后,肿块未见明显强化;
超声造影示(图6):胸膜下可见一大小约2.3 cm×2.1 cm的低回声肿块,经肘前静脉注射2.4ml对比剂声诺维,尾随5ml0.9%的生理盐水后,病灶呈“快进快出”强化表现。提示:胸膜占位,建议穿刺活检。行B超引导下肺穿刺,见黑色病理组织。病理结果示(图7):恶性黑色素瘤。
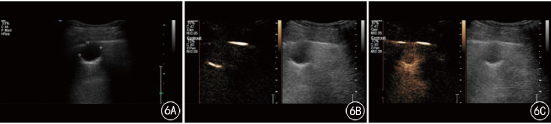
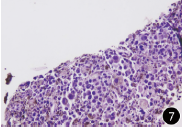
图6A~C超声造影:病灶呈“快进快出”强化表现;图7病理:细胞核异型明显,并见较多黑色素沉积(Envision二步染色法,×20)
讨论
黑色素瘤又叫恶性黑色素瘤,以皮肤黑色素瘤最为多见,皮肤外好发部位主要为眼、外阴,其次为直肠、肛门、生殖道、消化道、副鼻窦、腮腺等。原发于肺的黑色素瘤极为罕见,应用Pubmed、Web of Science及中国知网,输入(肺,原发,黑色素瘤)检索,结合文献总结,国内外报道均不足40例。肺的黑色素瘤以转移性为多,原发少见,文献称已公布严格的诊断标准,恶性黑色素瘤与支气管上皮细胞的变化有关。
Wilson等提出的诊断标准:(1)无皮肤、黏膜或眼部手术或电灼史;(2)孤立的肺肿瘤;(3)病理证实为恶性黑色素瘤;(4)诊断时未见其他任何部位的肿瘤。因此,完整的皮肤、眼、妇科等检查后,如果未发现原发性色素性病变,则支持原发性黑色素瘤的诊断。本例病变为右下肺下叶孤立性肿块,常规体检、妇科检查、腹部及浅表淋巴结超声、头颅CT等临床辅助检查均未发现肺外原发性黑色素瘤,病理诊断为黑色素瘤,符合原发性黑色素瘤诊断。黑色素瘤CT表现为软组织密度影,增强扫描强化欠均匀,不具备特征性。
CT对恶性黑色素瘤的定性有一定限度,但可清晰显示病变范围、部位、侵犯及骨质破坏情况,对临床确定治疗方案及判断预后有重要作用。本例病变边界清晰,密度较均匀,与胸膜及近侧肺血管关系密切,周围肺组织未见明显浸润性改变,相邻肋骨未见明显侵犯,增强后强化较均匀,与良性肺肿瘤无法区分。典型黑色素瘤因富含黑色素,MRI常表现为T1WI高信号,T2WI低信号。
本例肺黑色素瘤MRI表现典型,肿块边界清晰,抑脂T1WI序列为明显高信号,T2WI信号不均匀,病灶内见片状低信号区,为黑色素成分,并且DWI序列扩散明显受限,符合恶性肿瘤特征。黑色素瘤恶性程度很高,预后极差,现阶段尚未出现较好的治疗方法,手术和/或放、化疗后的生存期在14个月以内,但治疗手段仍以病灶在内的肺叶或全肺切除加周围淋巴结的清扫为主。
总之,肺原发性黑色素瘤极为罕见,诊断依据影像表现、病理特征及无其他部位原发病史。典型的黑色素瘤根据MRI表现即可确诊,肺部MRI的应用,可以明确肿块的位置、形态、大小、范围及与周围组织的关系,并能够显示肿块的性质,据此分析肿块的成分。对典型黑色素瘤的短T1、短T2信号显示清晰。并能观察不典型黑色素瘤内的黑色素成分及瘤内出血,根据其病理特征综合判断。若发现肺内结节或肿块,应考虑到该病的可能,并行MRI检查以为诊断提供更确切的依据。
原始出处:
卞巍,张敏鸣.肺原发黑色素瘤一例[J].临床放射学杂志,2019(03):400-401.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#色素#
17
#黑色素#
22
#黑色素#
15