Blood:维奈托克+利妥昔单抗治疗复发性CLL的长期疗效
2021-09-15 Nebula MedSci原创
维奈托克+利妥昔单抗可诱导复发性慢性淋巴细胞白血病患者获得持久的深度缓解
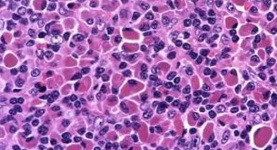
采用化学免疫疗法(CIT)初治治疗后获得深度缓解、微小残留病灶检测不到(uMRD)的慢性淋巴细胞白血病(CLL)患者在不继续治疗的情况下,也可具有延长的无进展生存期(PFS)。但是,在复发性或难治性(R/R)背景下,采用 CIT 治疗获得深度缓解的患者比例明显降低。
近日,《血液》期刊上报道了一项 1b期研究的长期随访结果,该研究旨在评估维奈托克和利妥昔单抗(VenR)用于复发性 CLL 患者的疗效。
在该研究中,受试患者接受维奈托克(200-600 mg/日)和利妥昔单抗持续治疗 6 个月后,该为维奈托克单药维持。经流式细胞术评估获得完全缓解(CR)、CR+不完全的骨髓恢复(CRi),或微小残留病灶阴性的患者可停止治疗(也可不停止),并且在进展时可重新采用 VenR 治疗。
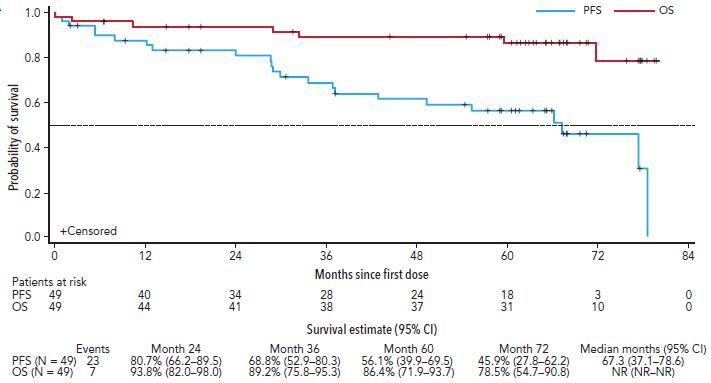
PFS 和 OS
共招募了 49 位患者,中位随访时间是 5.3 年。5 年总存活率、无进展生存率和缓解持续率分别是 86% (72-94)、56% (40-70)和 58% (40-73)。在 33 位获得了深度缓解(CR/CRi 或 uMRD)的患者中,有 14 位患者仍在进行维奈托克单药治疗(持续治疗),19 位患者在中位随访了 1.4 年后停止了维奈托克治疗(限期治疗)。
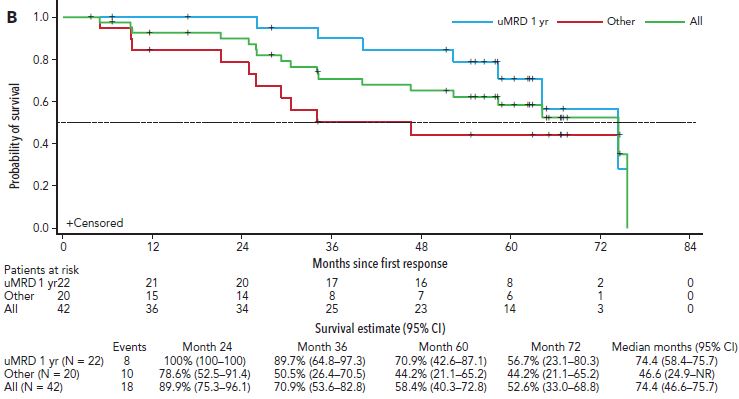
获得缓解的患者的缓解持续时间
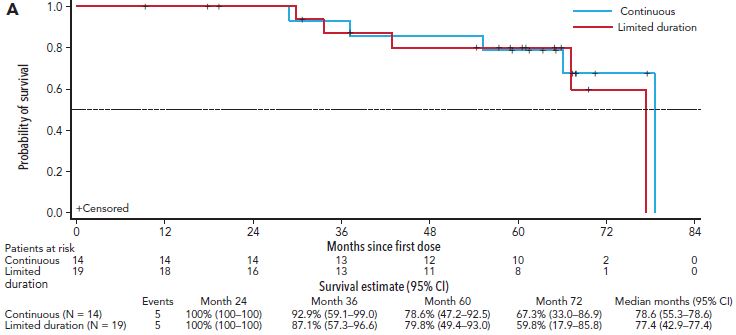
持续治疗或限期治疗患者的持续缓解率的五年估计值相近(71% vs 79%)。限期治疗组 19 位患者中有 6 位后续出现病程进展,都停用维奈托克超过两年(范围 2.1-6.4)。4 位患者重新进行了 VenR 治疗,截止评估日期,其中 3 位获得了部分缓解。
持续治疗或限期治疗患者的 PFS
综上所述,对于慢性淋巴细胞白血病患者而言,VenR 方案诱导的深度缓解,无论随后患者是持续治疗还是停止治疗都具有高度持久性。停止治疗后病程进展的 CLL 患者再用 VenR 诱导治疗仍可获得缓解。获得深度缓解的患者持续维奈托克治疗似乎不能增加额外的效益。
原始出处:
Shuo Ma, John F. Seymour, et al. Efficacy of venetoclax plus rituximab for relapsed CLL: 5-year follow-up of continuous or limited- duration therapy. Blood (2021) 138 (10): 836–846.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#利妥昔#
44
#复发性#
41
受益
70
#长期疗效#
45
学习了
79
学习了#学习#
62