Oncogene:重磅!乳腺癌预后差?这种药或许要早用!
2017-07-26 茨木 转化医学网
我们通常用抗雌激素疗法治疗雌激素受体阳性的乳腺癌,但其中约一半患者体内存在具有角蛋白CK5标志物的细胞亚群,并对治疗表现出耐药性——CK5表达越高的乳腺癌患者预后越差。这些特殊的细胞具有干细胞的特征,不仅能在治疗中残存,还能驱动甚至重启肿瘤生长。先前研究表明,人体内维生素A自然降解的产物维甲酸,具有对抗CK5 +细胞的作用,但将维甲类化合物应用于乳腺癌治疗的临床试验基本都已失败告终。 而科罗拉多
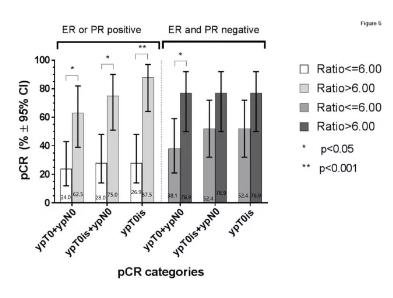
我们通常用抗雌激素疗法治疗雌激素受体阳性的乳腺癌,但其中约一半患者体内存在具有角蛋白CK5标志物的细胞亚群,并对治疗表现出耐药性——CK5表达越高的乳腺癌患者预后越差。这些特殊的细胞具有干细胞的特征,不仅能在治疗中残存,还能驱动甚至重启肿瘤生长。先前研究表明,人体内维生素A自然降解的产物维甲酸,具有对抗CK5 +细胞的作用,但将维甲类化合物应用于乳腺癌治疗的临床试验基本都已失败告终。 而科罗拉多大学(CU)癌症中心在线发表的一项最新研究,则强有力的解释了这些治疗失败的原因。同时,研究人员也提出了使用维甲酸及维甲类化合物治疗乳腺癌的有效策略。这项研究将刊印在Oncogene期刊上。研究表明,之前的临床试验主要是针对用过其他各种治疗方法的乳腺癌患者开展研究,癌细胞可能已经过了某个重要的临界点,所以产生了维甲酸药物抵抗。这就意味着,如果在治疗早期就使用维甲酸药物,则出现抗药性的可能会大大降低。虽然这种治疗策略未经过验证,但产生更好结果的可能性还是很大的。 最初的结论是通过研究雌激素和孕酮得出的,CU癌症中心的研究人员Carol Sartorius博士在先前的研究中发现孕酮具有帮助CK5 +细
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gene#
33
好办法,希望能治理好。
66
#重磅#
20
#Oncogene#
22
学习了,谢谢分享
72
学习了,涨知识
50
继续关注
74