肝癌是最常见的恶性肿瘤之一,中国不仅是肝癌大国,而且是世界第一肝癌大国。
根据国际癌症研究机构(IARC)2020年全球癌症负担数据,2020年全球新发癌症病例1929万例,中国新发癌症457万例。对于肝癌来说,全球2020年新发肝癌91万例,其中中国新发肝癌41万例,占全球45%还要多。
在全球肝癌死亡患者方面,中国也是全球第一。2020年全球肝癌死亡83万人,其中中国肝癌死亡39万人。
近日,美国密歇根大学的研究人员在" Cancers "期刊上发表了一篇题为" Impact of Histotripsy on Development of Intrahepatic Metastases in a Rodent Liver Tumor Model "的研究论文。

研究人员开发了一项非侵入式的声波抗癌技术,可以分解小鼠的肝脏肿瘤、杀死癌细胞并刺激免疫系统防止肿瘤进一步扩散,这一进步可能会改善人类的癌症预后。
具体来说,仅需破坏50-70%的肿瘤体积就能够显着地治疗肿瘤,小鼠的免疫系统能够清除其余部分,并且超过80%的动物没有复发或转移。
在该研究中,研究人员利用一种称为组织切除术(histotripsy)的治疗方法,以无创方式聚焦超声波,以毫米级精度机械破坏目标组织。
在许多临床情况下,由于肿块的大小、位置或阶段等原因,不能直接针对整个癌性肿瘤进行治疗。而这项技术有一种非常独特的优势,可以针对不同大小、位置和进展阶段的肿瘤都起效。
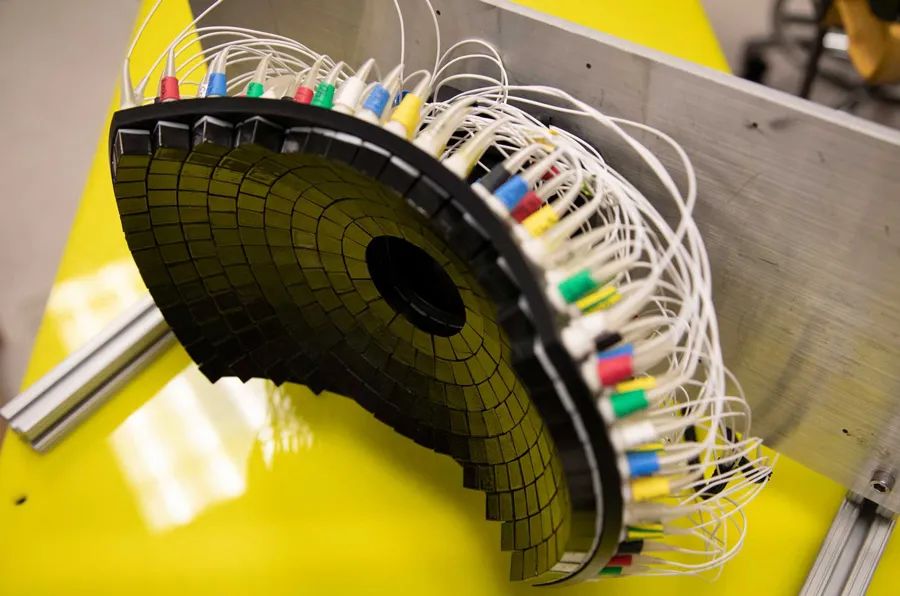
实验室中使用的超声阵列换能器
研究人员对22只小鼠植入了肝癌,将动物随机分为治疗组和对照组,11只小鼠接受部分组织切除术消融,靶向切除肿瘤体积的50%-75%。另外一半作为对照组,未接受任何治疗。
治疗后,研究人员分析了治疗的成功程度,并寻找进展、转移和免疫标志物的迹象。
研究发现,治疗组小鼠有9只(82%)表现出肿瘤消退,治疗中没有发现并发症和副作用,并在剩余的研究中经历了约10周的无瘤生存期。
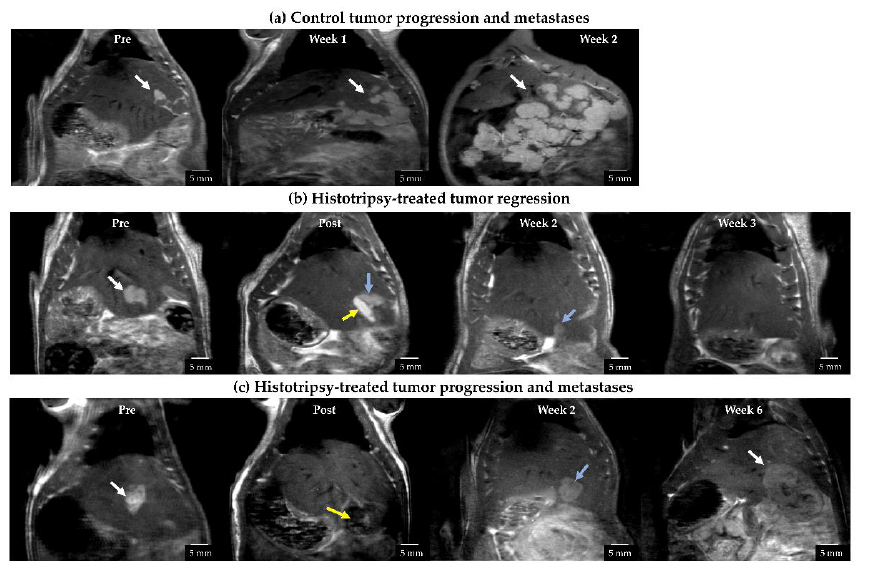
经组织切除术治疗(b)的肿瘤显示完全消退
而对照组小鼠的预后很糟糕,所有小鼠都显示出肿瘤进展和转移的迹象。在三周内,肿瘤达到伦理协议允许的最大尺寸,动物被安乐死。
研究人员表示,即使不针对整个肿瘤,仍然可以使肿瘤消退,并降低未来转移的风险。
结果还显示,这种治疗刺激了小鼠的免疫反应,也提高了治疗后的存活率,可能有助于最终消退肿瘤的非靶向部分并防止癌症进一步扩散。
总之,与对照组相比,这项组织切除术可能不会增加消融后发生转移的风险。未来的研究将继续研究组织切除术的安全性、有效性和生物学效应,以潜在地转化为临床。
目前,这种相对较新的技术正在美国和欧洲用于人类肝癌试验。
原始出处:
Tejaswi Worlikar, et al. Impact of Histotripsy on Development of Intrahepatic Metastases in a Rodent Liver Tumor Model. Cancers 2022, 14(7), 1612; https://doi.org/10.3390/cancers14071612.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ERS#
33
#根除#
41
好
49
#人体试验#
0