英国NICE否定了Zeposia治疗多发性硬化症的作用
2021-01-24 Allan MedSci原创
英国国家健康与护理卓越研究所(NICE)拒绝了百时美施贵宝(BMS)的Zeposia(ozanimod)用于治疗复发难治多发性硬化症(RRMS)的申请。
英国国家健康与护理卓越研究所(NICE)拒绝了百时美施贵宝(BMS)的Zeposia(ozanimod)用于治疗复发难治多发性硬化症(RRMS)的申请。

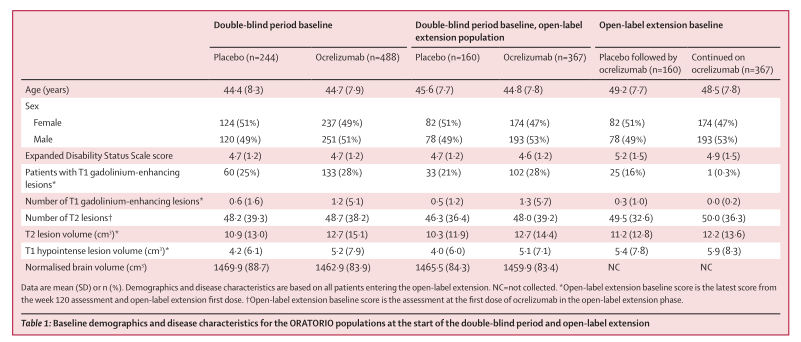
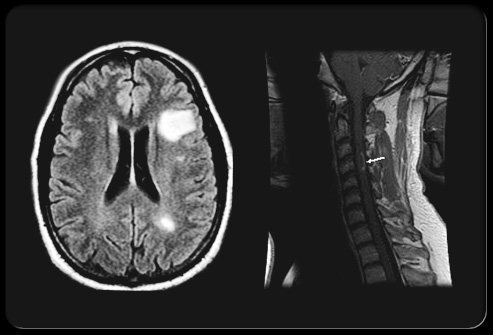
NICE在一份评估咨询文件中说,尽管有证据表明Zeposia与干扰素beta-1a相比可以减少多发性硬化症患者的复发次数和脑部病变,但尚不清楚该药物对残疾进展的影响。NICE还表示,由于临床有效性证据中存在“局限性”,因此不确定Zeposia的成本效益估算。
去年5月,Zeposia被欧洲药品管理局批准用于RRMS的治疗,并且去年还获得了美国食品和药品监督管理局(FDA)的批准。
MS协会研究和对外事务总监Sarah Rawlings说:“令人沮丧的是,NICE决定不建议使用Zeposia治疗MS。虽然针对这种情况有多种治疗方法,但口服型药物仍然很少,人们可以从一种新的,更方便的替代方案中受益匪浅。NICE的决定并非最终决定,我们敦促他们和制造商审查证据,并考虑哪种方法最适合MS患者”。
原始出处:
http://www.pharmatimes.com/news/nice_no_for_bms_multiple_sclerosis_drug_zeposia_1361753
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#硬化症#
36
#多发性#
34
#NICE#
43
#英国NICE#
49
唉
70
1
84