J Clin Oncol:卡培他滨维持 vs 治疗中断对一线治疗后病情稳定的转移性结直肠癌患者预后和生活质量的影响
2021-09-14 xiaozeng MedSci原创
接受姑息性化疗的转移性结直肠癌 (mCRC) 患者的治疗中断可减少毒性负担,改善生活质量 (QoL)
接受姑息性化疗的转移性结直肠癌 (mCRC) 患者的治疗中断可减少毒性负担,并可改善生活质量 (QoL)。虽然有大量随机试验证据表明,转移性结直肠癌患者使用治疗中断可在不影响总生存预期的情况下提高患者的生活质量。但目前的标准强制要求或推荐采用持续维持治疗,直到病情进展或不可耐受的毒性。
FOCUS4-N 研究旨在探索口服抗癌药维持治疗对一线治疗有反应的新确诊的转移性结直肠癌患者预后的影响。受试患者被1:1随机分成两组,接受卡培他滨维持治疗或接受积极监测(AM)。主要终点是无进展生存期(PFS),次要终点包括总生存期(OS)、毒性和耐受性。
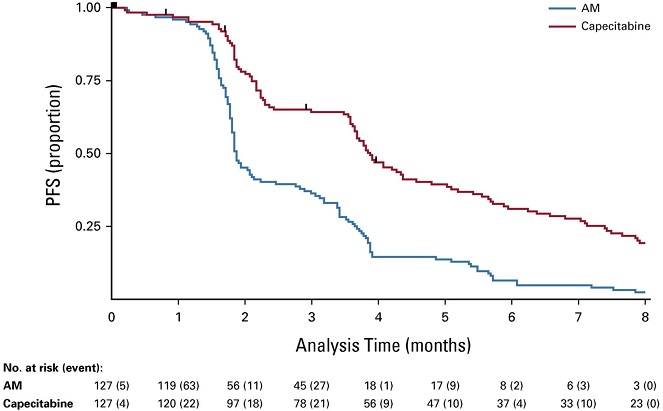
两组的中位无进展生存期
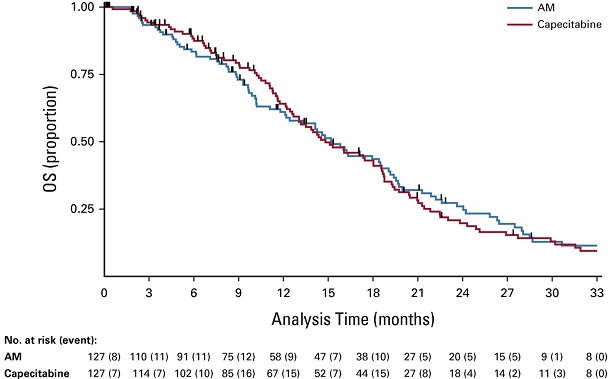
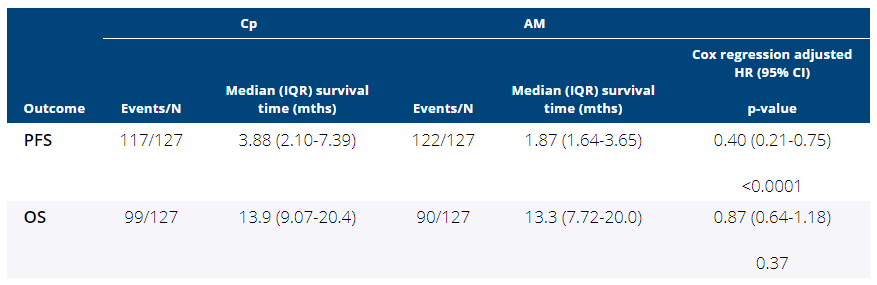
2014年3月至2020年3月期间,共招募了 254 位患者(卡培他滨组和 AM 组各 127 位)。两组患者的基线特征均衡。卡培他滨组和 AM 组的中位 PFS 分别是 3.88 个月和 1.87 个月,未校正的和校正的风险比(HR)分别是 0.44 (95% CI 0.33-0.57,p<0 .0001) 和 0.40 (95% CI 0.21-0.75, p<0.0001)。AM 组和卡培他滨组的 OS 无明显差异,中位 OS 分别是 15.2 个月 (95% CI 12.1-18.5) 和 14.8 个月 (95% CI 23.7-18.6),未校正的和校正的 HR 分别是 1.00 (95% CI 0.75-1.33, p=0.98) 和 0.93 (95% CI 0.69-1.27, p=0.66)。
两组的总生存期
治疗依从性良好,两组 2级及以上的毒性反应(卡培他滨 vs AM)有疲劳(25% vs 12%)、腹泻(23% vs 13%)和手足综合征(26% vs 3%)。两组间的生活治疗稍有差异。
虽然有强有力的证据表明维持治疗可以控制转移性结直肠癌患者的病情,但不能延长患者的总生存期。FOCUS4-N 试验提供了额外的证据,支持采用治疗中断作为对一线治疗有反应的或稳定的 mCRC 患者控制安全的替代选择。
原始出处:
Richard A. Adams, et al. Capecitabine Versus Active Monitoring in Stable or Responding Metastatic Colorectal Cancer After 16 Weeks of First-Line Therapy: Results of the Randomized FOCUS4-N Trial. Journal of Clinical Oncology. September 13, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.01436
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
28
#患者预后#
30
#治疗中断#
34
#病情稳定#
35
#病情#
28
#卡培他滨#
31
#转移性#
30
#结直肠#
29
学习#学习#
49
好好学习
59