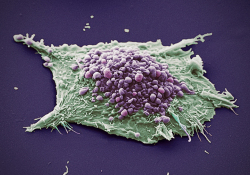
JNCCN:伴有前哨淋巴结(SN)阳性以及SN包膜结外延伸(ENE)的黑色素瘤患者的生存
2021-07-28 yd2015 MedSci原创
研究表明,ENE是前哨淋巴结(SN)阳性黑色素瘤患者的预后因素。这个指标有助于临床上筛选需要辅助化疗的患者。
在黑色素瘤患者中,前哨淋巴结(SN)阳性是识别高复发风险的重要指标,这些患者应作为辅助治疗的候选者。15%至20%的黑色素瘤患者可通过淋巴结活检(SNB)发现淋巴结转移。通常SN阳性患者会接受完全的淋巴结切除术(CLND),但是有研究表明CLND并不能改善患者的预后,因此不再推荐SN阳性患者进行CLND。近期有研究团队,评估SNs阳性黑色素瘤患者中SN包膜结外延伸(ENE)以外的黑色素瘤细胞的存在作为预后因素的价值,相关结果发表在Journal of the National Comprehensive Cancer Network杂志上。

研究纳入1047例患者,其中伴有ENE的有148 (14.1%)例,无ENE的有899 (85.9%)例。SNs阳性伴有ENE和不伴有ENE患者的中位随访时间分别为81个月和69个月。SNs阳性伴有ENE和不伴有ENE患者的5年的OS率分别为62.5% (95% CI, 54.3%-272.0%)和71.7% (95% CI, 68.3%-275.3%);而10年的OS率分别为47.5% (95% CI, 38.2%-259.1%)和60.8% (95% CI, 56.6%-265.3%)。

OS
SNs阳性伴有ENE和不伴有ENE患者的5年无病生存率(DFS)分别为54.0% (95% CI, 45.7%-263.8%)和64.0%(95% CI,60.5%-267.7%),而10年的DFS率分别为33.7% (95% CI,25.4%-244.8%)和45.2% (95% CI, 40.9%-249.9%)。两组的局部和区域复发的粗略累积发生率(CCIs)没有明显差异。但是在伴有ENE患者中,5年和10年远处转移的CCIs分别为31.8% (95% CI, 24.4%-241.4%)和 47.1% (95% CI, 38.2%-258.1%),而不有ENE患者中,5年和10年远处转移的CCIs分别为22.2% (95% CI, 19.3%-225.6%) 和 30.0% (95% CI,26.4%-234.2%),有统计学差异(p<0.001)。
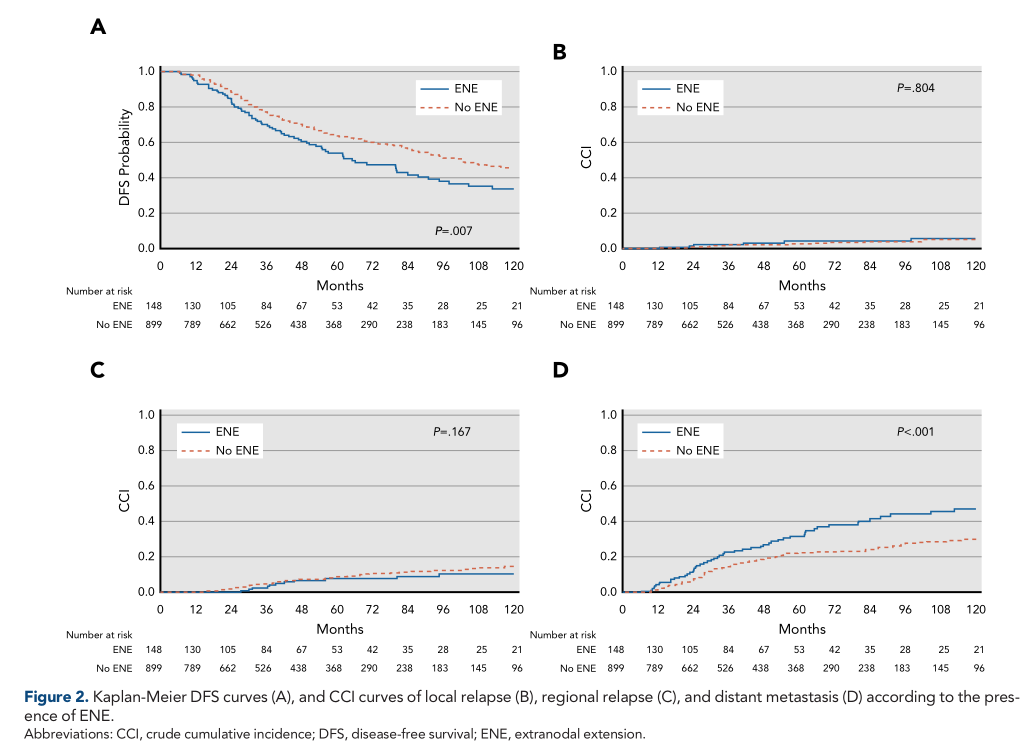
DFS
多因素分析,只有年龄(OR, 1.80; 95% CI, 1.272-2.56; P<0.001), SN主要转移灶的大小(OR, 9.99; 95% CI, 5.552-17.96;P<0.001), CLND后非SNs阳性的数目(p=0.001)跟ENE有关。
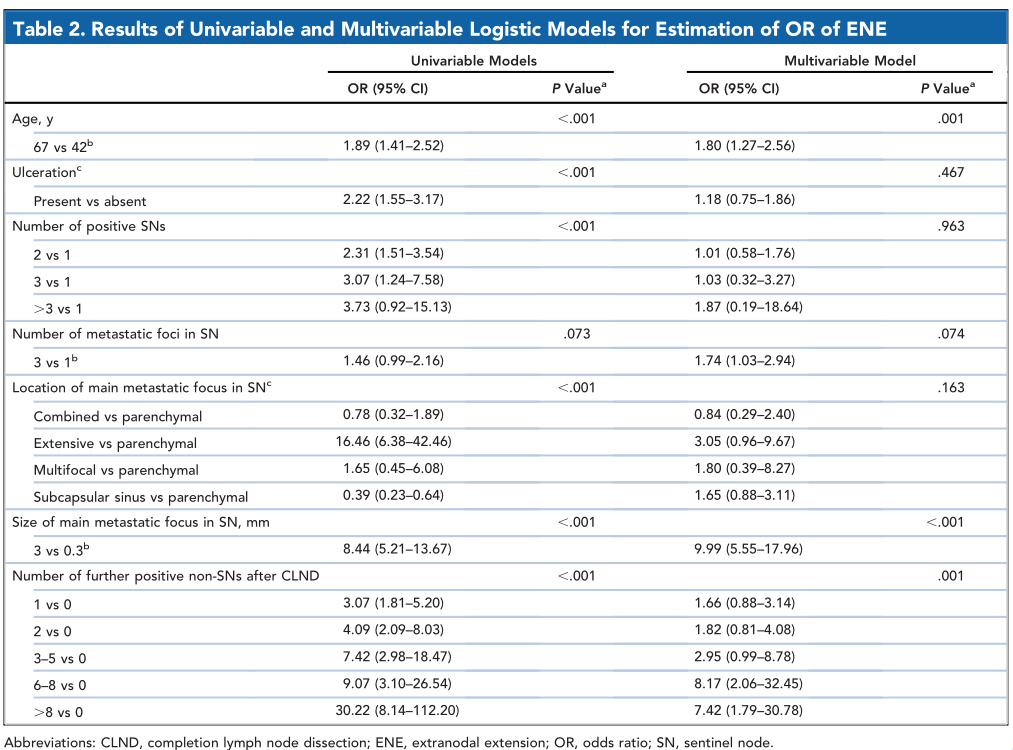
ENE相关因素
多因素Cox 回归模型分析发现,ENE、年龄、溃疡、SN主要转移灶的大小、非SN的转移灶数目是OS和DFS的预后因素(all p<0.001)。
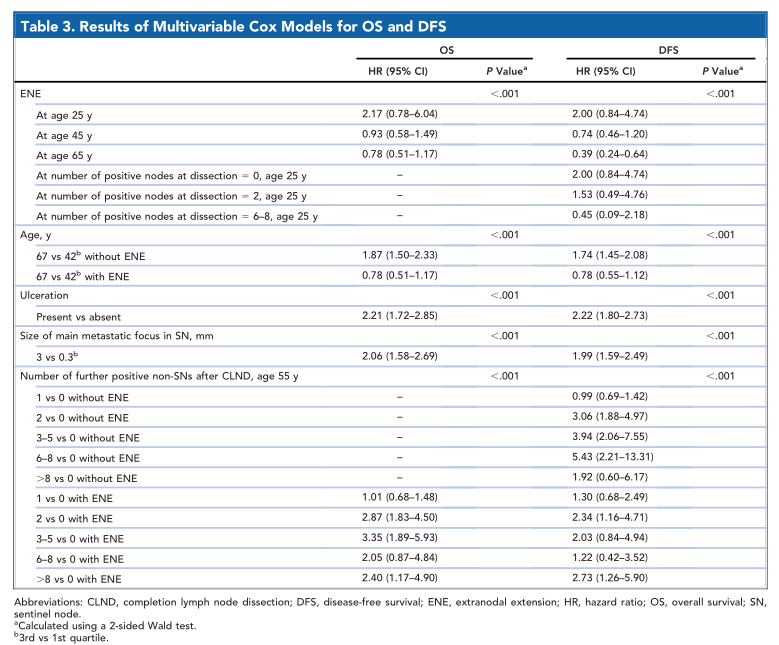
OS和DFS相关因素
综上,研究表明,ENE是前哨淋巴结(SN)阳性黑色素瘤患者的预后因素。这个指标有助于临床上筛选需要辅助化疗的患者。
原始出处:
Maurichi A, Barretta F, Patuzzo R, et al. Survival in Patients With Sentinel Node-Positive Melanoma With Extranodal Extension. J Natl Compr Canc Netw. 2021 Jul 26:jnccn20357. doi: 10.6004/jnccn.2020.7693. Epub ahead of print. PMID: 34311443.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#色素#
48
#淋巴结#
51
#NCCN#
54
#前哨淋巴结#
63
#黑色素#
50
#黑色素#
39
目前黑色素瘤的整体发病率不高,企业研究成功的药品并不一定能赚回成本
73