丙种球蛋白是一种广泛表达和分泌的生长因子,在多个生物过程中发挥作用,包括神经回路发育、细胞生长调节、伤口愈合、溶酶体平衡和神经炎症。丙种球蛋白是由位于17q21.31号染色体上的GRN基因编码的。该基因的杂合突变是额颞叶变性(FTLD)的第二大常见原因,占所有FTLD病例的10%。这些功能缺失的GRN突变导致丙种球蛋白的单倍体功能不足,随后出现溶酶体功能障碍和神经变性。
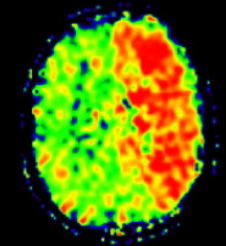
 图1: 论文封面图
图1: 论文封面图
最近,全基因组关联研究发现GRN基因座内的常见变异与其他年龄相关的神经退行性疾病有关,如阿尔茨海默病和帕金森病。此外,对携带致病性GRN变体的患者进行的神经病理学研究发现,除了预期的TDP-43阳性内含物外,还经常出现路易体共病,这表明路易体疾病和额颞叶痴呆之间存在潜在的分子联系。
有趣的是,在路易体痴呆(LBD)病例中已经有罕见的偶然GRN突变的报道,但这些观察结果的相关性仍不清楚。
藉此, 美国NIH的Neurodegenerative Diseases Research Unit的Paolo Reho等人,基于这些先前的证据推测GRN突变可能引起LBD。核心目的是评估一个LBD病例对照队列中GRN的致病变体,并测试LBD患者中是否有丰富的破坏性变体。
他们分析了2591个欧洲血统的LBD病例和4032个神经系统健康的对照对象产生的全基因组测序数据,以确定GRN的致病突变。
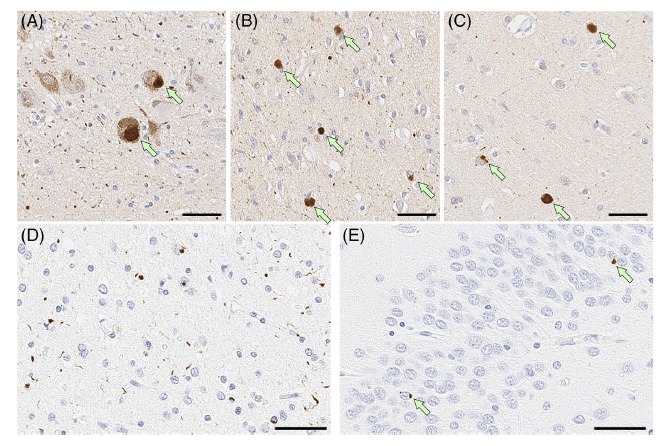
图2:论文结果图
他们在7名研究参与者中发现了6个杂合的GRN外显子突变(病例:n = 6;对照组:n = 1)。每个变体都被预测为致病或可能致病。
而且,与对照组相比,LBD患者的GRN功能缺失突变明显富集(优化序列核心关联测试P = 0.0162)。
三个明确的LBD病例的免疫组化显示了路易体病理学和TDP-43阳性的神经元内含物。
该研究表明,有害的GRN突变是家族性LBD的一个罕见原因。
原文出处:
Reho P, Koga S, Shah Z, et al. GRN Mutations Are Associated with Lewy Body Dementia. _Movement Disorders_. Published online July 10, 2022:mds.29144. doi:[10.1002/mds.29144](https://doi.org/10.1002/mds.29144)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Disord#
52
#disorder#
48
#路易体#
47
#ERS#
39
#disorders#
36
#Dis#
24
学习,学习
36
学习学习学习学习学习学习学习学习学学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习习学习
44
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
33