Clin Neuropharm:阿立哌唑用于创伤后应激障碍
2017-10-29 佚名 大话精神
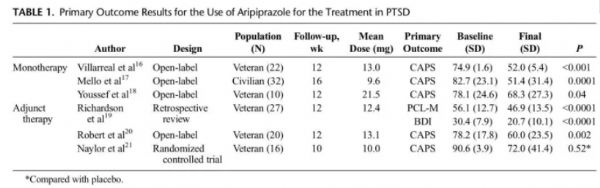
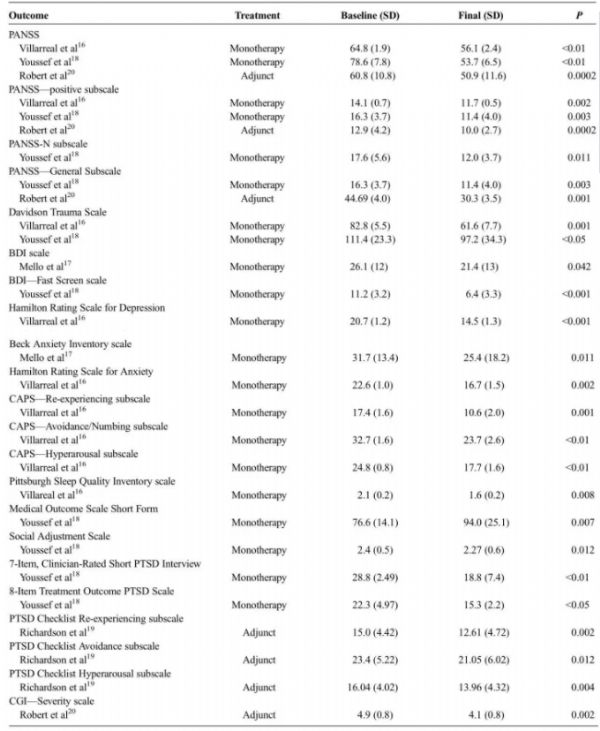
创伤后应激障碍(PTSD)是一种精神病性症状,常常在一个人经历或见证某种煽动恐惧,无望或恐怖感受的创伤事件或压力源之后发展。它可能很快发生,也可能在事件发生后很长时间才出现。PTSD药物治疗主要是选择性5-羟色胺再摄取抑制剂(SSRIs),目前FDA批准的两种SSRI为帕罗西汀和舍曲林。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Pharm#
39
#创伤#
37
#阿立哌唑#
42
#应激#
36
谢谢分享.
47
继续关注.
38
继续学习.
44