J Autoimmun:系统性红斑狼疮患者左心室大小和功能与狼疮抗凝剂相关:超声心动图随访研究
2022-09-02 MedSci原创 MedSci原创
该研究发现狼疮抗凝剂(LAC)的存在与5年随访期间的舒张功能测量以及进行性左心室(LV)扩张有关。因此,LAC可能是 SLE患者心功能不全的预测因子。
系统性红斑狼疮(SLE)是一种慢性自身免疫性疾病,心脏功能障碍的风险增加。病理生理机制知之甚少,预后标志物是必要的。该研究的目的是在5年的随访期间确定与心脏大小和功能测量相关的SLE特征。
研究人员纳入了108名SLE患者:90%为女性,平均年龄46±13 岁,中位病程14年(范围 7-21)。在基线和5年随访时对潜在的生物标志物进行了血液采样以及标准超声心动图检查。为了研究超声心动图参数与基线和未来5年变化的关联,对SLE相关基线变量(临床疾病活动、狼疮性肾炎、慢性肾病、抗心磷脂和/或抗β-2糖蛋白I抗体和狼疮抗凝剂(LAC))进行了多变量回归分析并针对传统风险因素进行了调整。
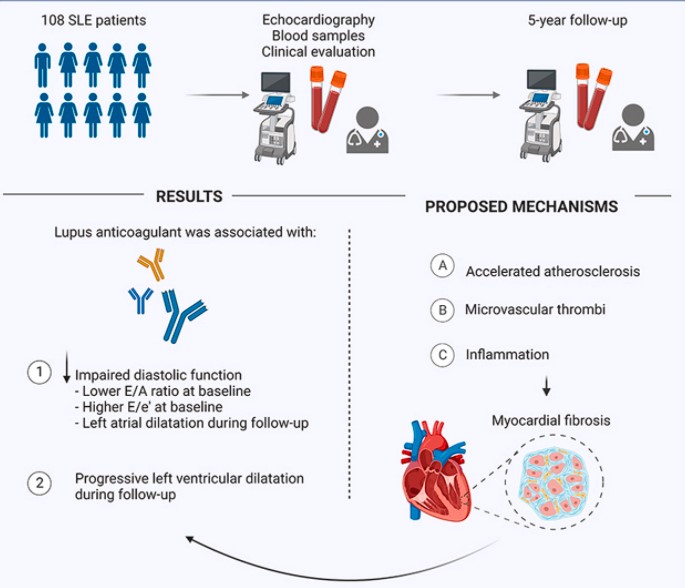
在随访期间,五分之二的超声心动图测量舒张功能退化(E/A比1.4±0.5 vs. 1.3±0.5,p = 0.002;三尖瓣反流峰值速度2.0±0.6 vs. 2.2±0.4 mmHg,p < 0.001 )。左心室(LV)舒张末期容积指数增加(43.7±13.9 vs. 52.5±15.7 mL/m2, p < 0.001)。左右心室收缩功能保持稳定。LAC与舒张功能差相关:基线时E/A比值较低(p = 0.04)和E/e'比值较高(p = 0.04),随访期间左心房容积指数增加(p = 0.01)。在随访期间LAC与LV扩张进一步相关(p = 0.01)。
该研究发现LAC的存在与5年随访期间的舒张功能测量以及进行性LV扩张有关。因此,LAC可能是 SLE患者心功能不全的预测因子。已知LAC对微血管循环有影响,但目前研究结果的临床意义尚待阐明。
出处:Myhr KA, Zinglersen AH, Hermansen MF, Jepsen MM, Iversen KK, Ngo AT, Pecini R, Jacobsen S. Left ventricular size and function in patients with systemic lupus erythematosus associate with lupus anticoagulant: An echocardiographic follow-up study. J Autoimmun. 2022 Aug 24;132:102884. doi: 10.1016/j.jaut.2022.102884. Epub ahead of print. PMID: 36029716.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#随访研究#
43
#系统性#
52
#心动图#
57
学习
55
#狼疮#
36
#左心室#
53
#红斑#
39