JAHA:加利福尼亚州妊娠相关心肌梗死的发病率和机制变化
2021-10-22 MedSci原创 MedSci原创
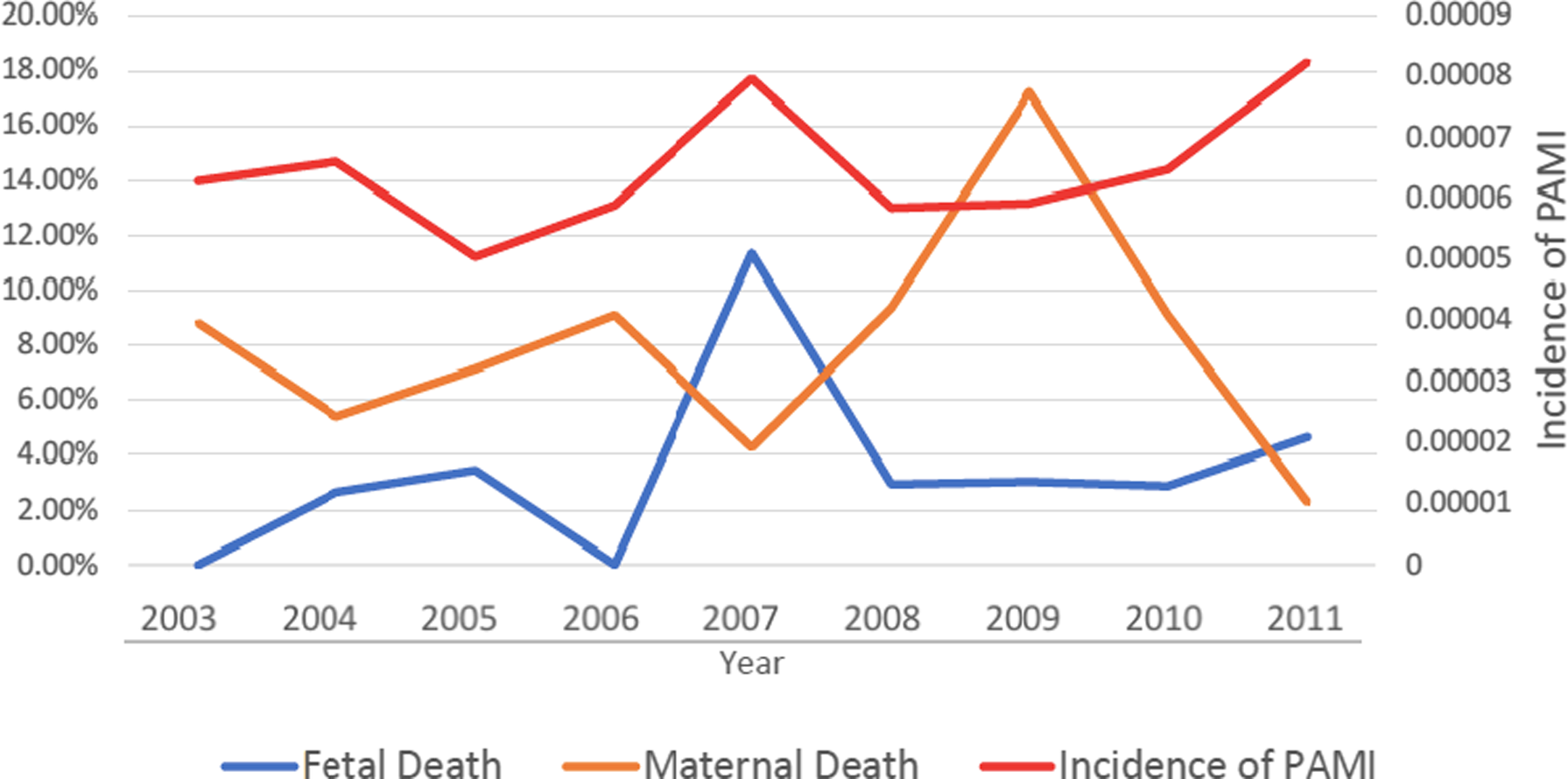
在过去的十年中,加利福尼亚州的PAMI发病率呈上升趋势,自发性冠状动脉夹层、血管痉挛和Takotsubo综合征的发病机制呈上升趋势。这些结果值得进一步调查。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在评估加利福尼亚州妊娠相关心肌梗死(PAMI)的时间趋势,并探索潜在的危险因素和发病机制。

研究人员采用加利福尼亚州住院患者数据库分析了2003年至2011年期间国际疾病分类第九修订版(ICD-9)代码为妊娠或产后急性心肌梗塞入院患者;并对危险因素进行了分析,且与未发生心肌梗死的妊娠患者进行比较。

研究人员总共从5266380次妊娠(每100000次妊娠中发生6.5次)中确定了341名PAMI患者。PAMI患者住院孕产妇死亡率为7%,婴儿死亡率为3.5%。从2003年到2011年,PAMI发病率没有显著增加的趋势,这可能是由于自发性冠状动脉夹层、血管痉挛和Takotsubo综合征的发生率较高。
与未患心肌梗塞的孕妇相比,PAMI对年龄较大(72% vs. 37%,P<0.0005)、黑人(12% vs. 6%,P<0.00005)、年龄大于30岁、较低的社会经济地位(最低四分位数的家庭收入中位数为26% vs. 20%,P=0.04),较高的高血压患病率(26% vs. 7%,P<0.0005),糖尿病(7% vs. 1%,P<0.0005),贫血(31% vs. 7%,P<0.0001)、使用苯丙胺(1% vs. 0%,P<0.00005)、可卡因(2% vs. 0.2%,P<0.0001)和吸烟(6% vs. 1%,P=0.0001)相关。
由此可见,在过去的十年中,加利福尼亚州的PAMI发病率呈上升趋势,自发性冠状动脉夹层、血管痉挛和Takotsubo综合征的发病机制呈上升趋势。这些结果值得进一步调查。
原始出处:
Sawan Jalnapurkar.et al.Changing Incidence and Mechanism of Pregnancy‐Associated Myocardial Infarction in the State of California.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021056
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发病率#
31
学习
52
#AHA#
36
不错不错
82