IBD: 万古霉素可有效治疗溃疡性结肠炎患者的慢性储袋炎症
2022-04-13 xuyihan MedSci原创
溃疡性结肠炎(Ulcerative Colitis)是一种局限于结肠粘膜及粘膜下层的炎症过程。病得多位于乙状结肠和直肠,也可延伸至降结肠,甚至整个结肠。病理漫长,常反复发作。
溃疡性结肠炎(UC)患者行回肠-肛门吻合术(IPAA)后极易出现储袋炎症,储袋炎是治疗UC的IPAA后最常见的并发症。虽然急性储袋炎的使用抗生素治疗作为一线治疗方法已相对明确,但慢性炎症的抗生素治疗方法仍不确定。接受直肠切除术和IPAA治疗UC的患者中,约有50%的人将会发展成慢性储袋炎。尽管大多数患者对一线抗生素治疗有反应,但仍有高达19%的患者会发展为慢性储袋炎。慢性肠袋炎对生活质量有很大的负面影响,口服万古霉素是一种全身吸收较差的抗生素,作为单药治疗不仅对储袋炎患者有效,而且对UC和原发性硬化性胆管炎(PSC)患者的亚组也有效。因此,本项研究旨在评估万古霉素在治疗慢性储袋炎相关疾病方面的有效性。
为此,研究人员收集了北卡罗来纳大学(UNC)多学科炎症性肠病治疗中心接受治疗的患者的数据。通过卡罗莱纳州健康数据库识别接受过万古霉素治疗的储袋炎的患者。万古霉素的剂量为125毫克,每天两次,口服。典型的储袋炎症状包括尿频、尿急、尿失禁或腹泻腹痛。对万古霉素的临床反应的定义是基于在开始治疗4周后是否仍然需要抗生素治疗。
研究结果显示有41名患者因慢性储袋炎症而接受了万古霉素治疗。这些人中,54%是女性,85%是白人。在使用万古霉素之前,这些患者平均使用了3.98种抗生素,在开始使用万古霉素4周后,21名患者(51%)表现出临床反应。在3个月和6个月的持久性评估中,21名应答者中的16名(76%)表现出持续的应答,并继续服用慢性病药物,在20名患者中在4周时没有表现出初步反应,对于这部分患者研究人员比较了4周后出现临床反应的患者的内窥镜PDAI分值的变化,没有明显的差异。
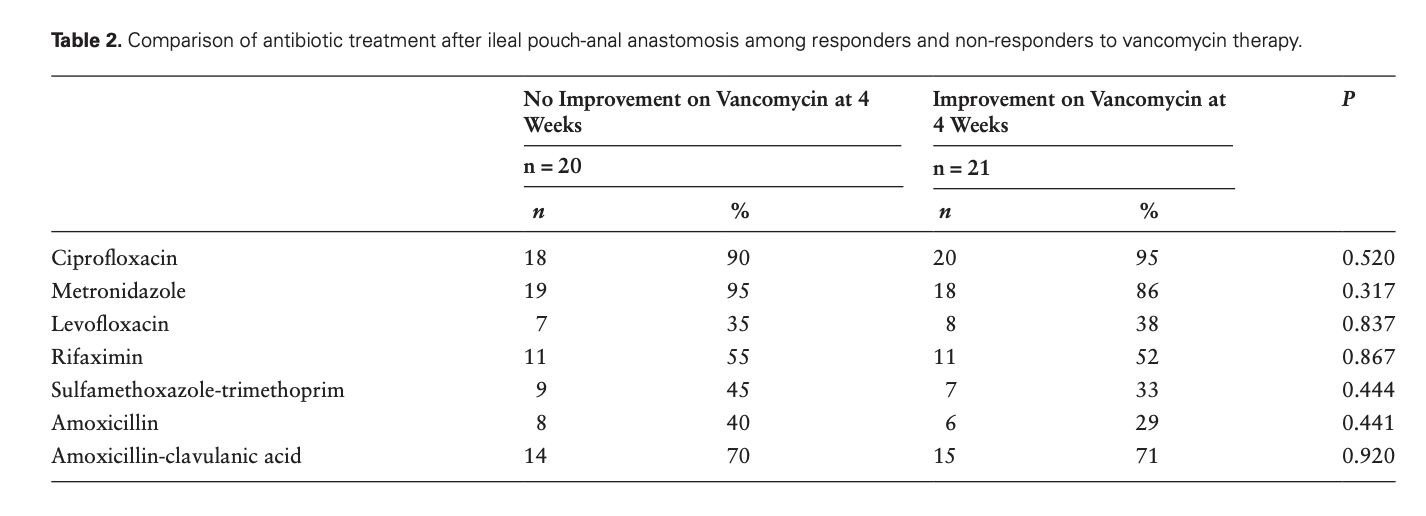
图:不同抗生素对于慢性储袋炎的治疗效果
本项研究证实在对万古霉素治疗慢性储袋相关疾病疗效的回顾性分析中,研究人员发现大约一半的患者在 4 周时表现出临床反应。此外,76% 的反应者在 3 个月和 6 个月时继续表现出临床反应。
原始出处:
Gabriel Lupu. Et al. Vancomycin Is Effective in the Treatment of Chronic Inflammatory Conditions of the Pouch. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#溃疡性#
40
#IBD#
48
#治疗溃疡性结肠炎#
47
#有效治疗#
54