IBD: 组织学炎症活动和类固醇使用史是溃疡性结肠炎患者临床复发的危险因素
2022-05-03 xuyihan MedSci原创
溃疡性结肠炎是一种病因尚不十分清楚的结肠和直肠慢性非特异性炎症性疾病,病变局限于大肠黏膜及黏膜下层。
溃疡性结肠炎 (UC) 是一种特发性慢性炎症性肠病,其特征是结肠黏膜或黏膜下层炎症,并倾向于累及结肠远端。UC 治疗的目标是通过使用适当的治疗来改变自然病程并避免长期肠道损伤和致残性并发症的出现。因此,识别高危患者对于这种慢性疾病至关重要。最近,UC 的治疗靶点已从控制症状转向内镜缓解。内镜下愈合与更好的长期结果相关,包括降低临床复发、住院、结肠切除术和结肠炎相关肿瘤形成的风险。临床试验中评估黏膜愈合最常用的工具是 Mayo 内窥镜评分 (MES),目前共识中将内窥镜愈合 (EH) 定义为 MES≤1。然而,对于是否所有 MES≤1 的患者都处于真正的黏膜愈合状态存在疑问。目前,黏膜愈合不能仅通过内窥镜的视觉外观来评估。组织学愈合的新概念已成为治疗目标,UC 中组织学愈合的患者表现出更好的预后和更低的类固醇使用率和住院率。因此,本研究旨在根据梅奥内窥镜评分 (MES) 为 0 或 1 的 UC 组织学活动来评估临床复发的风险。

研究人员回顾性分析了在其医疗中心就诊的 UC患者的临床资料,所有患者均行活检粘膜检查,最后总共有492 名 MES 为 0 或 1 的 UC 患者被纳入并分析。主要观察结果是临床复发的发生,其主要定义为包括在随访期间药物治疗、住院、结肠切除术的变化以及结直肠癌的出现。
在中位 549 天的随访期间,92名(18.7%)UC患者出现临床复发。所有患者均更换药物治疗,其中住院患者4例。Geboes 评分≥3.1(风险比 [HR],1.732;P = . 035)和类固醇使用史(HR,1.762;P=. 008)定义的组织学活动是与临床复发相关的独立因素。进一步分层分析后,研究人员发现组织学改善且无类固醇使用史的患者的1年和2年临床复发率分别为4.1%和10.6%,而有组织学活动和类固醇使用史的患者的复发率分别为 23.9% 和 39.4%。
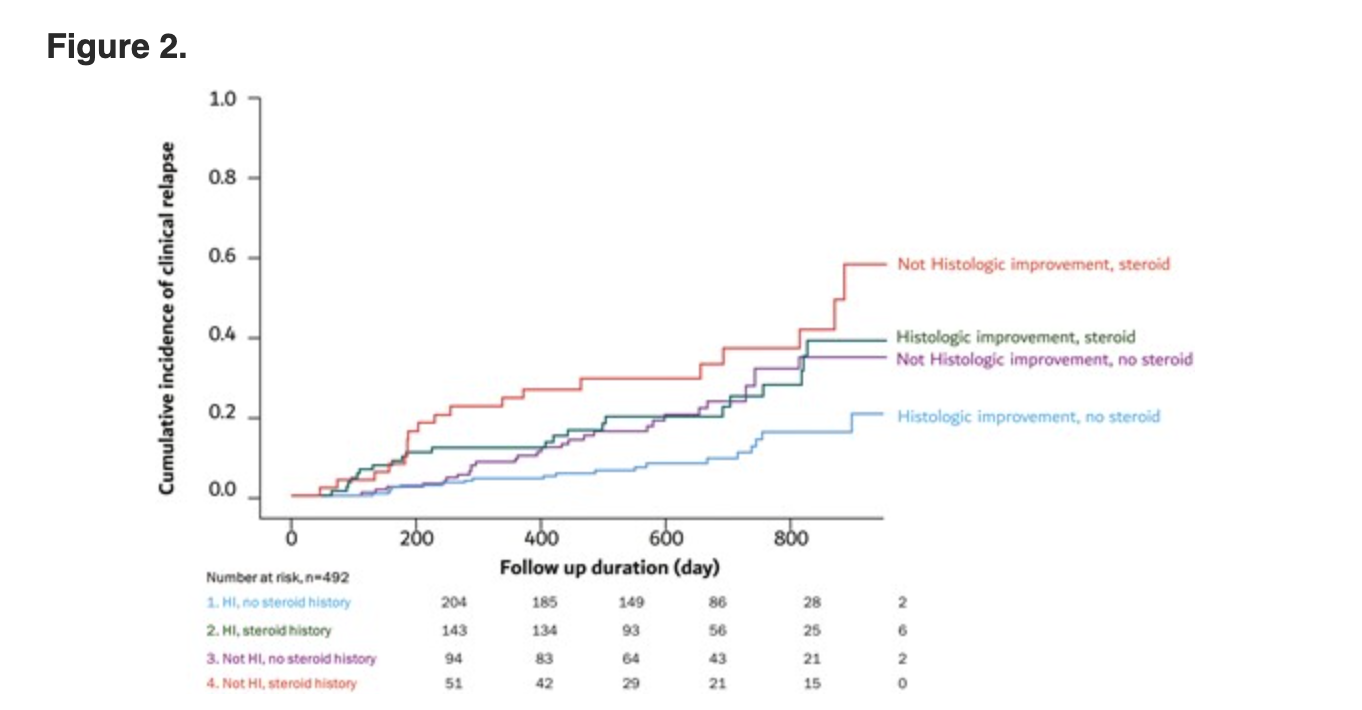
本项研究证实在 MES 为0或1的UC患者中,组织学炎症活动和类固醇使用史是UC患者临床复发的危险因素。
原始出处:
Gyeol Seong. Et al. Histologic Activity and Steroid Use History Are Risk Factors of Clinical Relapse in Ulcerative Colitis With Mayo Endoscopic Subscore of 0 or 1. Inflammatory Bowel Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#溃疡性#
31
#组织学#
36
#IBD#
43
#类固醇#
43