Nat Med:为何部分炎症性肠病患者对治疗没有反应?
2021-10-23 haibei MedSci原创
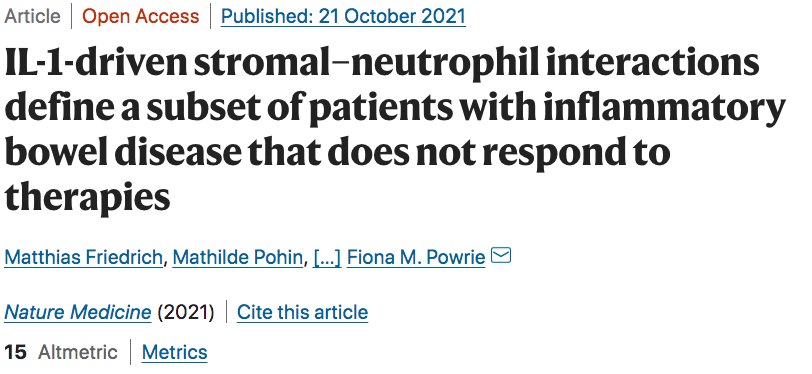
研究人员在三个IBD患者队列中(总人数=376)确定了IBD异质性组织炎症反应中共同表达的基因模块,这些基因模块映射到不同的组织病理学和细胞特征(病理类型)。
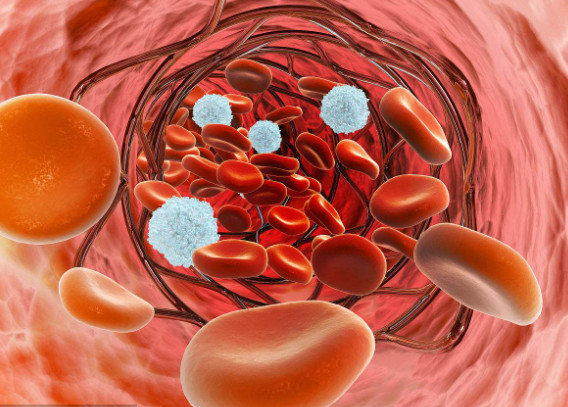
炎症性肠病是一组异质性疾病,以整个胃肠道的炎症为特征。病因涉及宿主与其肠道微生物群之间的不适应,这种互作由遗传和环境因素所控制。IBD的复杂性反映在其临床表型上,包括克罗恩病(CD)和溃疡性结肠炎(UC),以及一系列的微观特征,如肉芽肿、淋巴细胞聚集、隐窝脓肿和溃疡。
目前,IBD的治疗方法包括一般的免疫抑制剂(如皮质类固醇)、免疫调节剂(如硫嘌呤)或调节特定炎症介质的生物制剂(如抗肿瘤坏死因子-α,TNF-α)。然而,确定哪些患者会对治疗有反应仍然是一个重大挑战。
已有的研究发现,IL-6家族成员oncostatin M(OSM)及其受体OSMR的基因在IBD患者发炎的肠道中高表达,与抗TNF治疗无反应有关。值得注意的是,由白细胞产生的OSM信号主要进入基质细胞,如成纤维细胞和内皮细胞。随后的转录组研究将成纤维细胞、炎症性单核吞噬细胞(MNPs)、中性粒细胞和致病性T细胞以及浆细胞的亚群与UC和CD的治疗无反应相关。
目前,治疗反应的细胞和分子标志是否在不同患者中是统一的,或者几个不同的组织病理学是否通过不同的机制与治疗失败有关,这一点仍然是未知的。对这些领域的进一步了解对于设计个性化的治疗方案和对目前方案没有反应的个体的新疗法至关重要。
最近,结合混合和单细胞转录组学、定量组织病理学和原位定位,研究人员在三个IBD患者队列中(总人数=376)确定了IBD异质性组织炎症反应中共同表达的基因模块,这些基因模块映射到不同的组织病理学和细胞特征(病理类型)。
与患者对多种不同IBD疗法无反应有关的炎症基因共表达特征。
这些病理类型之一是由高中性粒细胞浸润、成纤维细胞激活和深溃疡部位的血管重塑所定义的。溃疡床的活化成纤维细胞显示出中性粒细胞的化学诱导特性,这与IL-1R有关,但与TNF无关。
在四个独立的队列中,与病理类型相关的中性粒细胞和成纤维细胞特征在对几种疗法没有反应的人中有所增加(总人数=343)。
因此,识别不同的、局部的、组织的病理类型将有助于当前治疗方法的精确定位,并为IL-1信号阻断在溃疡病中的应用提供生物学依据。
原始出处:
Matthias Friedrich et al. IL-1-driven stromal–neutrophil interactions define a subset of patients with inflammatory bowel disease that does not respond to therapies. Nature Medicine (2021).

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Nat#
35
学习的,非常感谢
61
#炎症性#
29
#炎症性肠病患者#
39
#Med#
37