JACC:生物瓣置换术后的瓣膜结构变化
2020-05-18 MedSci原创 MedSci原创
生物瓣置换术后常常出现亚临床小叶血栓形成,用四维计算机断层成像显示小叶增厚(HALT)和小叶运动减弱(RLM)。本研究的目的是确定主动脉生物假体置换术后HALT和RLM的频率、预测因子、血流动力学和临
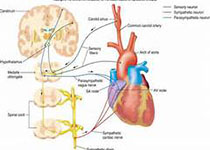
生物瓣置换术后常常出现亚临床小叶血栓形成,用四维计算机断层成像显示小叶增厚(HALT)和小叶运动减弱(RLM)。本研究的目的是确定主动脉生物假体置换术后HALT和RLM的频率、预测因子、血流动力学和临床相关性。
本研究纳入分析了Evolut临床研究中的没有接受口服抗凝治疗的经导管主动脉瓣置换术(TAVR)和外科主动脉瓣置换术患者。术后30天,HALT在TAVR组的发生率为17.3%,在外科组中为16.5%,RLM的发生率分别为14.6%和14.3%。术后1年,HALT在TAVR组和外科组患者的发生率分别为30.9%和28.4%,RLM的发生率分别为31%和27%。主动脉瓣血流动力学状态在两个时间点均不受HALT或RLM的存在或严重程度的影响。
研究结果显示,自扩式经导管主动脉瓣置换术后1年内,主动脉生物瓣的ct影像表现常有异常,但呈动态变化,但这些发现与低手术风险患者主动脉瓣置换术后的主动脉瓣血流动力学状态无关。
原始出处:
Philipp B et al.Bioprosthetic Aortic Valve Leaflet Thickening in the Evolut Low Risk Sub-Study.2020 May.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#置换#
32
#生物瓣#
40
#JACC#
33
#ACC#
34
#置换术#
29
#瓣膜#
34