JAHA:ST段抬高型心肌梗死患者神经肽Y水平与冠状动脉微血管功能、心力衰竭和死亡率的关系
2022-07-04 MedSci原创 MedSci原创
ST段抬高心肌梗死后,外周静脉和冠状静脉窦NPY水平与微血管功能和梗死面积相关。外周静脉NPY水平与随后的心衰发展或死亡率相关,因此它可能是一个有用的预后标志。
对于ST段抬高型急性心肌梗死患者,当前的目标是通过首次经皮冠状动脉介入治疗(PPCI)对梗死相关的心外膜血管进行快速血运重建,以恢复冠状动脉灌注。交感共传递素神经肽Y(NPY)在ST段抬高心肌梗死时释放到冠状动脉窦,并可收缩冠状动脉微血管。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员试图明确容易获得和测量的外周静脉NPY水平是否与微血管阻塞、心肌恢复和预后相关。
研究人员对接受首次经皮冠状动脉介入治疗的患者立即测定NPY水平,并与血管造影和心血管磁共振微血管功能指标进行比较。
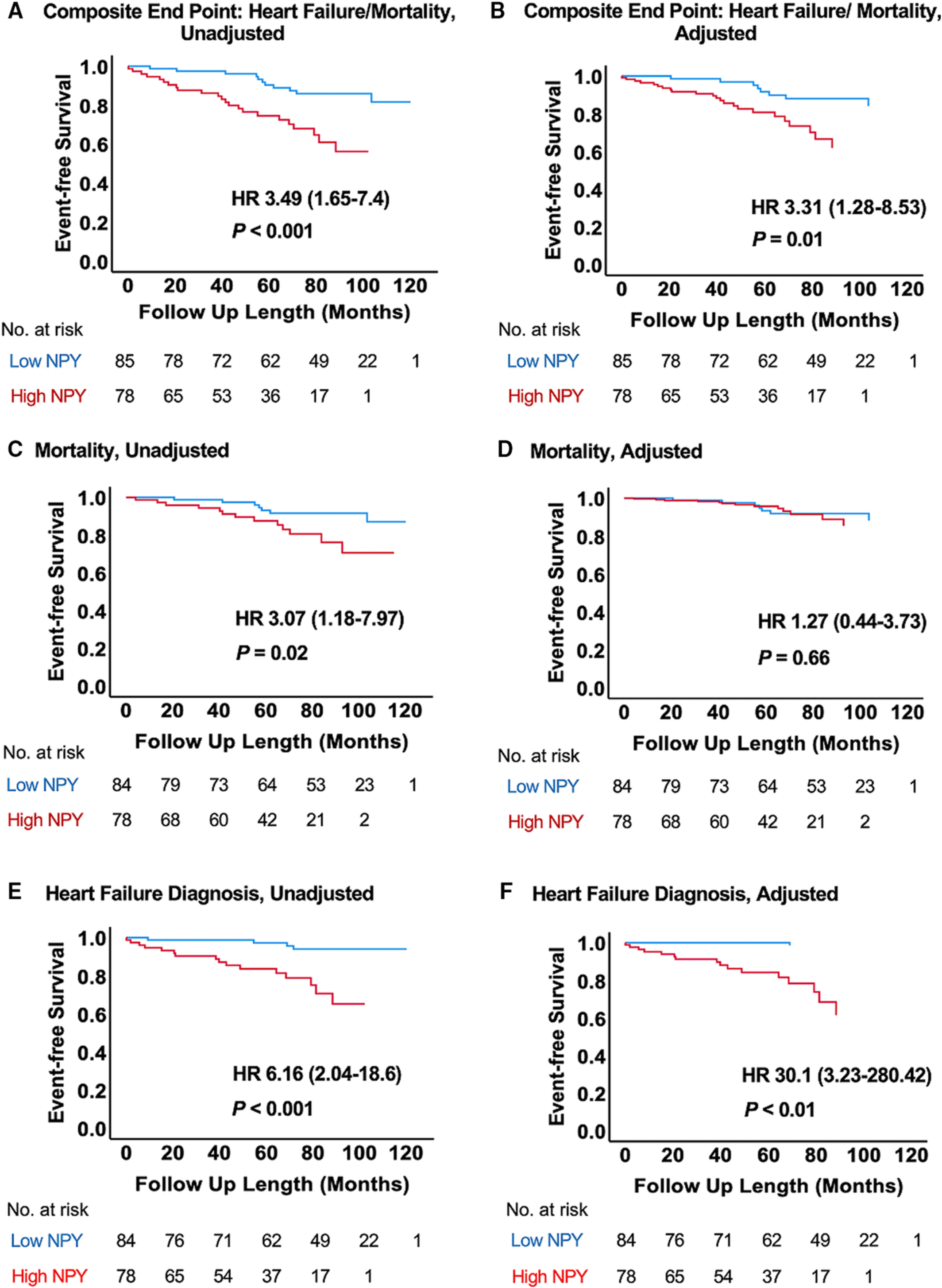
受试者前瞻性地随访6.4年(四分位差范围为4.1-8.0年)。外周静脉(n=163)与冠状窦(n=68)NPY水平呈显著相关(r=0.92;P<0.001),与多种冠脉及微血管功能和梗死面积的影像学参数(如冠状动脉血流储备、急性心肌水肿、左室射血分数和6个月后钆增强晚期)相关。因此,研究人员在随访期间评估了外周静脉NPY的预后价值,其中34例(20.7%)患者发生心力衰竭或死亡。Kaplan-Meier生存分析显示,高外周静脉NPY水平(经二元递归划分,>21.4pg/mL)与心力衰竭发生率和死亡率增加相关(风险比为3.49[95%CI为1.65-7.4];P<0.001)。在调整了年龄、心血管危险因素和以前的心肌梗死后,这种关联仍然保持不变。
由此可见,ST段抬高心肌梗死后,外周静脉和冠状静脉窦NPY水平与微血管功能和梗死面积相关。外周静脉NPY水平与随后的心衰发展或死亡率相关,因此它可能是一个有用的预后标志。需要进一步的研究来验证这些结果。
原始出处:
Thomas Gibbs.et al.Neuropeptide‐Y Levels in ST‐Segment–Elevation Myocardial Infarction: Relationship With Coronary Microvascular Function, Heart Failure, and Mortality.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.024850
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AHA#
38
#微血管#
41
#ST段抬高#
49
#血管功能#
45
#ST段#
48