重磅!阜外专家将携中国原创技术QFR新成果登上TCT舞台
2017-10-29 佚名 今日循环
10月29日~11月2日,全球介入心脏病学顶级学术会议TCT2017将在美国丹佛召开。大会最新研究的发布历来都是最受瞩目的重头戏,值得中国学者骄傲的是,10月31日,中国原创技术 QFR(定量血流分数)的临床验证研究FAVOR II China将在大会主会场作为First Report Investigation首次发布,由中国医学科学院阜外医院徐波教授带来精彩报告。
10月29日~11月2日,全球介入心脏病学顶级学术会议TCT2017将在美国丹佛召开。大会最新研究的发布历来都是最受瞩目的重头戏,值得中国学者骄傲的是,10月31日,中国原创技术 QFR(定量血流分数)的临床验证研究FAVOR II China将在大会主会场作为First Report Investigation首次发布,由中国医学科学院阜外医院徐波教授带来精彩报告。据悉,该研究论文已被心血管权威期刊JACC接收。这不仅意味着国际心血管领域对QFR临床价值的极大认可,也意味着QFR推向临床应用又迈出了坚实的一步。
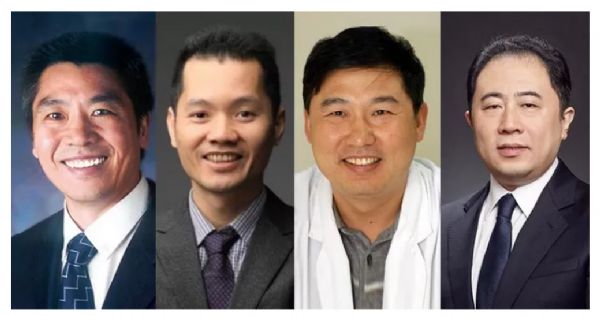
FAVOR II China主要研究者
中国医学科学院阜外医院胡盛寿院士、QFR技术发明者上海交通大学涂圣贤博士、
FAVOR II China共同主要研究者阜外医院乔树宾教授和徐波教授
仅用造影数据即可精确快速计算FFR的中国原创技术
在冠脉介入治疗技术日益成熟和广泛开展的今天,准确评估病变狭窄程度与心肌缺血的关系、借助冠脉功能学评价指导介入治疗的重要性日益凸显。冠脉血流储备分数(FFR)是近年来用于判断冠状动脉临界病变是否需要进行血运重建的一种重要有效工具,但由于其有创性、操作较复杂以及压力导丝费用高等问题,导致全球、尤其是在我国FFR的临床应用受限。
在此背景下,基于影像的无创FFR计算技术成为近年来国际心血管领域备受关注的热点技术。QFR(Quantitative Flow Ratio),即定量血流分数测量系统,是由上海交通大学涂圣贤博士团队研发的具有自主知识产权的国产创新医疗设备,已于2017年5月由中国国家药监局特别审批为创新医疗器械。
QFR在国际上首次实现了介入导管室中无需压力导丝、患者无需注射腺苷或ATP,仅使用冠状动脉造影数据即可精确快速计算出FFR。QFR的早期临床结果已在JACC介入子刊上发表了2篇原创文章,其临床价值得到国内外专家的认可。
QFR的极简理念,从10分钟到30秒的再升级
QFR技术的研发经历了两个阶段:第一个阶段的研究成果于2014年发表在JACC: Cardiovascular Interventions。当时,涂圣贤博士团队创新性地尝试开发可以取代基于压力导丝检测的FFR技术,提出QFR的第一代技术,即FFRQCA技术。
FFRQCA在计算流体力学分析时采用了一种新的边界条件,将计算时间压缩到十分钟左右;同时,FFRQCA利用了常规冠脉造影中造影剂充盈血管过程所反映的个体化血流信息,提供了更准确的边界条件,提高了计算模型的诊断精度。
第二阶段的研究成果于2016年再次发表于JACC: Cardiovascular Interventions。经过临床应用的不断探索,导管室在线实时分析时,十分钟计算时间仍然相对较长,操作仍比较复杂,患者体验较差。
因此涂圣贤团队开始了第二个阶段的研发,提出了全新的计算模型,将计算时间从10分钟进一步降低至30秒内,加上影像传输、分析流程等总分析时间约4分钟,并且只需要常规造影而不需要使用微循环扩张药时也可进行FFR计算,这项升级的技术被称之为QFR技术。
FAVOR II China:从离线到实时,在临床实践中经受考验
前期已发表的临床研究均是离线在实验室进行分析,而QFR的最佳临床意义是导管室在线实时使用,以实现术中开展QFR评估指导介入手术的临床价值。
因此,中国医学科学院阜外医院牵头组织了FAVOR II China的临床研究,同时有四家分中心(中国人民解放军总医院、北京大学第三医院、上海胸科医院、广东省人民医院)联合参与,由阜外医院胡盛寿院士担任主要研究者,乔树宾教授和徐波教授担任共同主要研究者;于2017年7月完成病例入组。
FAVOR II China研究以FFR为金标准,评估在线实时QFR对具有血流动力学意义的冠脉狭窄诊断的一致性。
同期,FAVOR II Europe/Japan临床研究也已完成入组,其研究结果也将于TCT期间发布。
QFR技术已连续两年(2016~2017)共4次分别在中国介入心脏病学大会(CIT)、欧洲介入心脏病学大会(EuroPCR)的实况转播中,向全球展示QFR在线评估狭窄病变功能学意义及指导支架植入术方面的应用;得到EuroPCR大会主席William Wijns教授和英国Andreas Baumbach教授等国际一流学者的一致高度评价;认为QFR将是导管室非常有意义的革新工具,使医生可以在手术一开始就制定最正确、也是对病人最有利的治疗方案。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#新成果#
28
#TCT#
34
#重磅#
35
谢谢分享.超厉害的说
80
非常好.谢谢分享
84