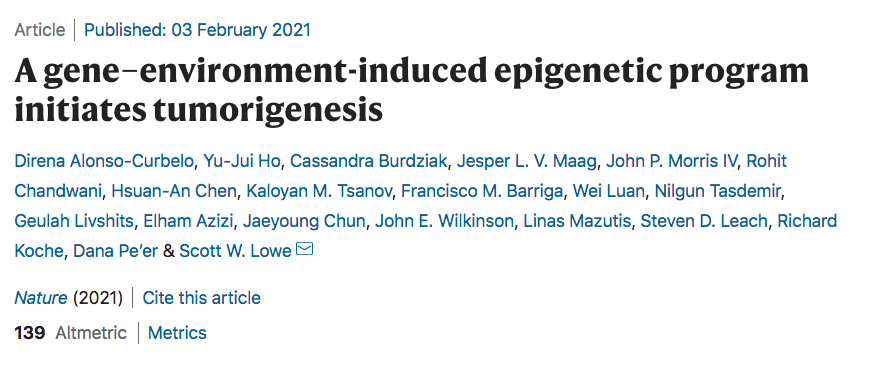
Nature:基因和环境共同诱导表观遗传程序,启动肿瘤发生
2021-02-04 haibei MedSci原创
在胰腺前上皮细胞组织损伤后最迅速激活的因子中存在报警素细胞因子白细胞介素33,它再现了损伤与突变的Kras合作的效果,以释放早期肿瘤和肿瘤转化的表观遗传重塑程序。
已有的研究显示,组织损伤会增加癌症的风险,但是我们对于其背后的机制还不甚了解。在小鼠胰腺癌模型中,与组织损伤相关的胰腺炎与Kras癌基因的激活突变合作,可以显著加快早期肿瘤病变的形成,并最终引发腺癌。
最近,研究人员在Nature杂志发文,其在自体小鼠模型中,通过整合基因组学,单细胞染色质测定和时空控制的功能扰动,表明Kras突变和组织损伤的组合在胰腺上皮细胞中促进了一个独特的染色质状态,以区别于正常的细胞再生。
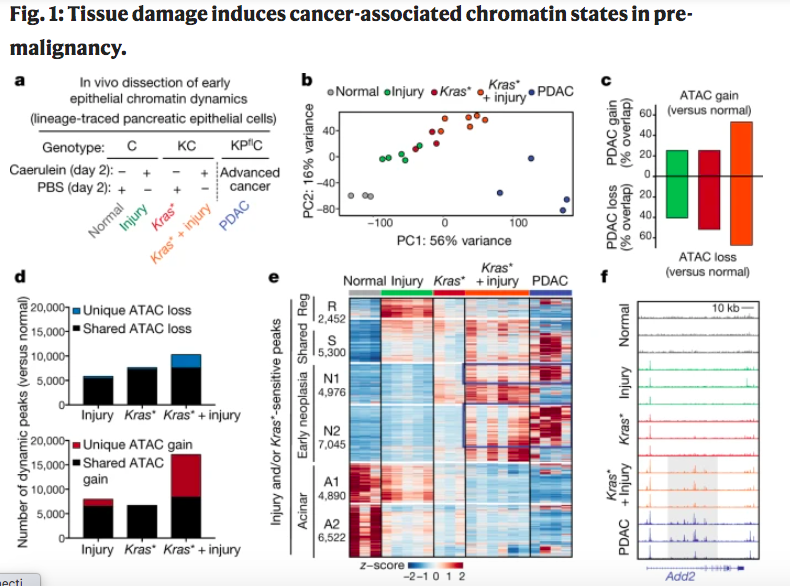
这种与癌症相关的表观遗传状态在胰腺损伤后48小时内出现,并涉及一个 "尖细胞到新生儿 "的染色质开关,有助于定义人类胰腺癌基因的早期失调。
在胰腺前上皮细胞组织损伤后最迅速激活的因子中存在报警素细胞因子白细胞介素33,它再现了损伤与突变的Kras合作的效果,以释放早期肿瘤和肿瘤转化的表观遗传重塑程序。
总的来说,该研究阐明了基因-环境的相互作用是如何迅速产生基因调控程序,决定早期肿瘤的转化,并提供了一个分子框架,来理解癌症启动中遗传和环境线索之间的相互作用。
原始出处:
Direna Alonso-Curbelo et al. A gene–environment-induced epigenetic program initiates tumorigenesis. Nature (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
33
已读,受益匪浅
88
高校博士科研团队,提供SCI论文科研服务,文章提供原始数据,作者审核文章内容及结果后投稿,可指定拟投杂志,文章接受后付款,前期不收任何费用。术业有专攻,期待与您的合作1615858451
83
#肿瘤#肿瘤相关研究是人类进步的见证!
108