J Heart Lung Transplant:REVEAL Lite 2风险评分可预测肺动脉高压患者的预后
2021-12-23 Nebula MedSci原创
REVEAL Lite 2 评分与肺动脉高压患者的生存预后和临床无恶化生存期相关
风险评估在肺动脉高压 (PAH) 的管理中是必不可少的。REVEAL 风险评分(RRS)已被证明可以预测 PAH 患者的生存预后,并在一系列风险评估中具有预后价值。近期,研究人员开发了一个更新版本(RRS 2.0),以进一步完善 PAH 患者的风险预测。
利奥西呱(Riociguat)是一种可溶性鸟苷酸环化酶(SGC)的刺激物,被用于治疗两种形式的肺动脉高压(PH):慢性血栓栓塞性肺动脉高压(CTEPH)和肺动脉高压(PAH)。
REVEAL Lite 2 评分是 REVEAL 风险评分的一种简易版。本研究旨在评估利奥西呱对REVEAL Lite 2 评分的影响,以及其与 PAH 患者长期预后的相关性。
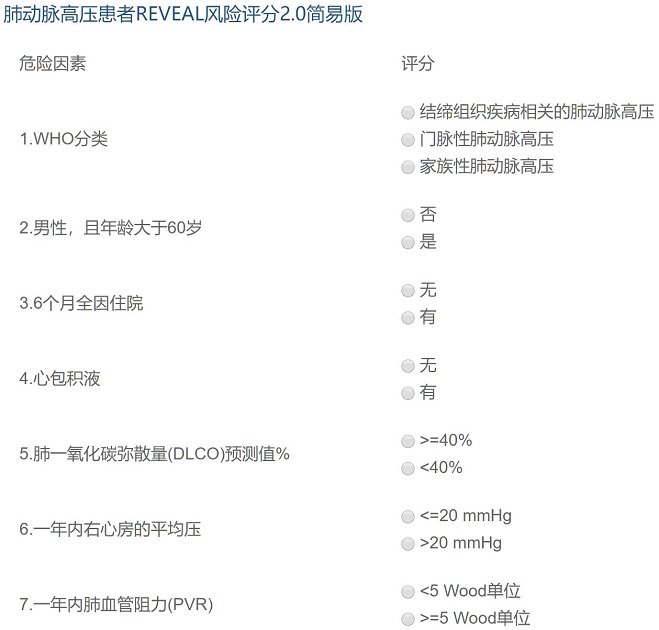
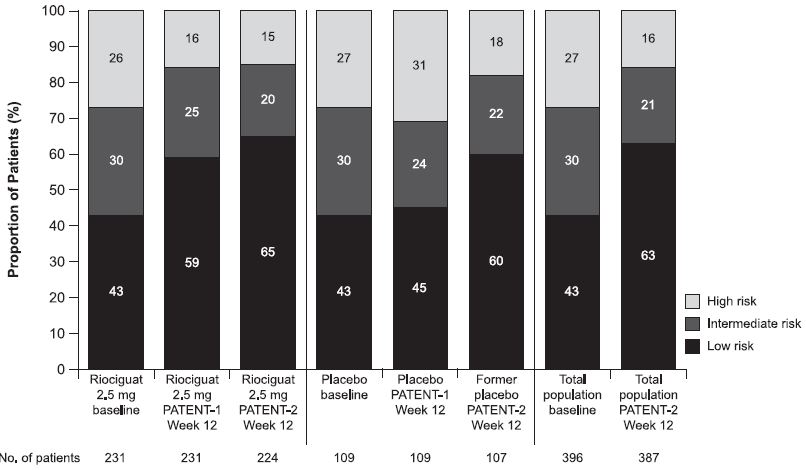
PATENT-1 是一项随机、双盲的临床试验,对比了 PAH 患者使用利奥西呱或安慰剂干预治疗的预后。在 PATENT-2 开放标签的扩展研究中,所有患者(n=396)每天接受利奥西呱(高达2.5 mg,3次/日)治疗。在基线、PATENT-1 第12周和 PATENT-2 第12周分别计算患者的 REVEAL Lite 2 评分;将患者分成了低(1-5分)、中(6-7分)或高风险(≥8分)层。
不同时间点低、中、高 REVEAL Lite 2 评分患者占比
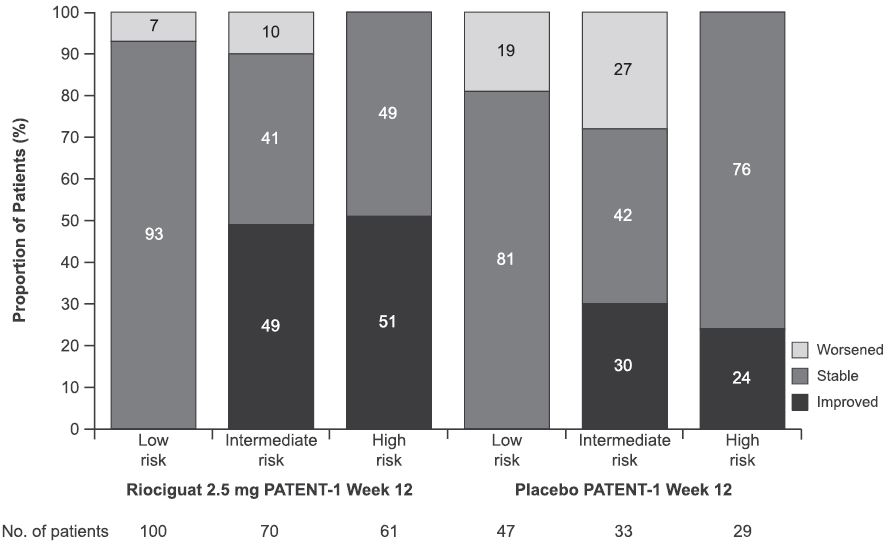
PATENT-1 第12周时,接受利奥西呱 2.5 mg治疗的患者的 REVEAL Lite 2 评分有所改善(与安慰剂相比的最小二乘均差 -0.8;p=0.0004)。在 PATENT-1 第12周时,与安慰剂相比,更多的接受利奥西呱 2.5 mg治疗的患者的风险层保持稳定或有所改善(p=0.0005)。
利奥西呱 2.5 mg vs 安慰剂治疗后REVEAL Lite 2 评分的变化
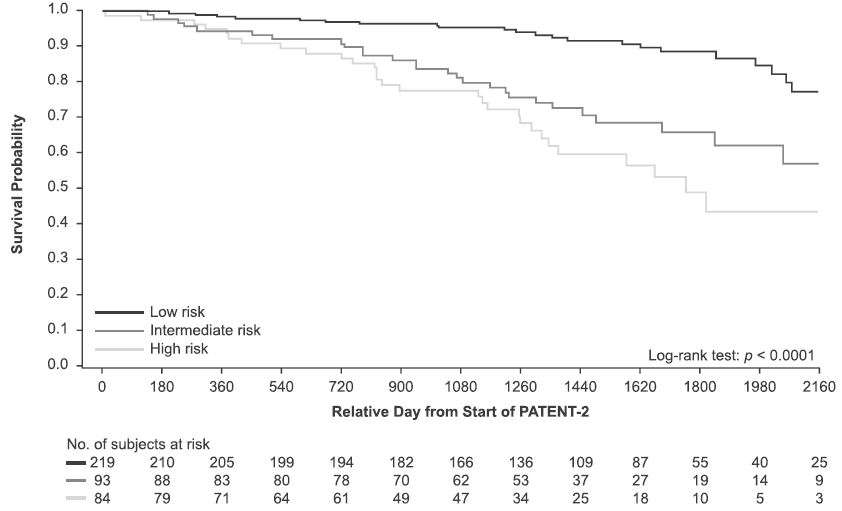
基线和 PATENT-1 第12周时的 REVEAL Lite 2 评分均与生存预后和临床无恶化生存期相关(p<0.0001),从基线到第12周时的评分变化也有如此相关性。基线和 PATENT-1 第12周时不同风险层之间的患者的生产率和临床无恶化生存均存在一定差异(p<0.0001)。
根据PATENT-1 第12周时的 REVEAL Lite 2 评分分组患者的生存率
综上所述,该研究表明利奥西呱可降低肺动脉高压患者的不良预后风险,并有助于进一步验证 REVEAL Lite 2评分在 PAH 风险评估中的应用。
原始出处:
Benza Raymond L,Boucly Athéna?s,Farber Harrison W et al. Change in REVEAL Lite 2 risk score predicts outcomes in patients with pulmonary arterial hypertension in the PATENT study.[J] .J Heart Lung Transplant, 2021, https://doi.org/10.1016/j.healun.2021.10.013
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#plant#
44
#肺动脉高压患者#
43
#TRA#
24
#Transplant#
47
#动脉高压#
0
#ART#
31
#HEART#
28