TAG:炎症性肠病患者使用维多珠单抗后粪便钙卫蛋白是内镜和组织学缓解的早期预测指标
2021-01-17 MedSci原创 MedSci原创
维多珠单抗-Vedolizumab(VDZ)是一种抑制α4β7整联蛋白的肠道选择性人源化单克隆抗体,目前已经被FDA批准用于治疗溃疡性结肠炎(UC)和克罗恩病(CD)的成年患者。
维多珠单抗-Vedolizumab(VDZ)是一种抑制α4β7整联蛋白的肠道选择性人源化单克隆抗体,目前已经被FDA批准用于治疗溃疡性结肠炎(UC)和克罗恩病(CD)的成年患者。但目前如何判断炎症性肠病患者(IBD)早期对于药物应答的效应和在内镜下疾病缓解程度目前还没有公认的方法。粪钙卫蛋白(FC)为IBD治疗期间监测粘膜改善情况和用于预测疾病复发的有用替代标记。有研究显示IBD患者接受VDZ治疗后体内粪便钙卫蛋白水平再26周显著下降,因此,本项研究旨在评估早期粪便钙卫蛋白(FC)是否可以预测VDZ治疗后的IBD患者的内窥镜反应和组织学缓解情况。

这是一项前瞻性研究。纳入标准为IBD患者存在内镜下炎症和FC>100 µg/g。在基线和第2、4、8和16周检测患者FC水平。在第16周,进行回肠和结肠活检的内窥镜检查。通过Wilcoxon Rank Sum检验评估FC变化。ROC统计数据用于评估FC的诊断准确性。
本项研究共纳入了45例IBD患者[27克罗恩病(CD),16/2溃疡性结肠炎(UC)/ IBD未分类] 。第16周内镜反应和组织学缓解率分别为58%和33%。在第8周时,FC <250 µg / g可以预测UC和CD的内镜反应(阳性预测值100%),而在第8周时,FC下降的情况与CD内镜反应的发生率无关[阴性预测值(NPV)82% ],与UC和CD均无组织学缓解(NPV 90%)相关性。
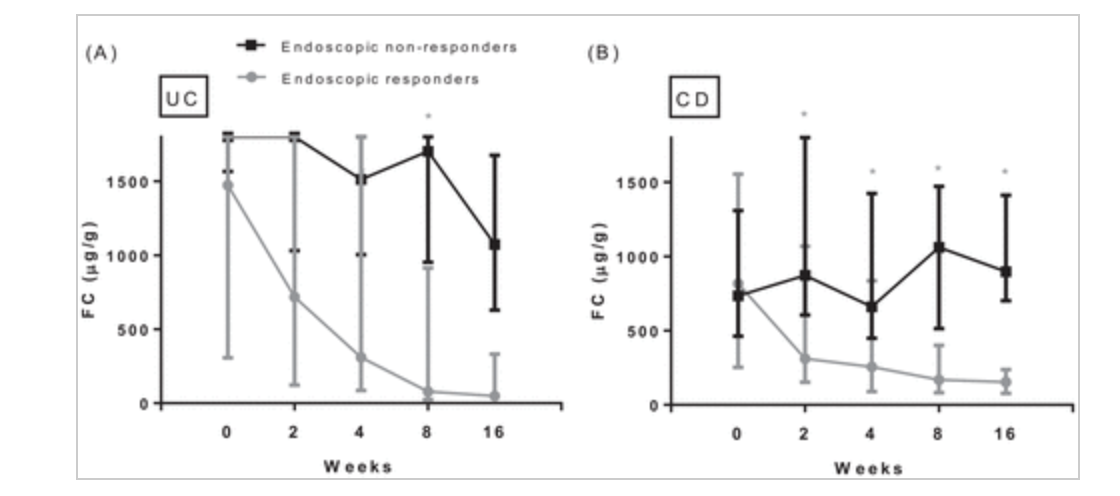
因此,通过本项研究发现,在第8周时,FC <250 µg / g与内镜反应有关,而在第8周时,FC的下降程度与内镜反应和组织学缓解均无关。VDZ开始后8周的FC水平可用于指导临床决策,并可替代内窥镜检查,更加方便。
原始出处:
Renske W. M. Pauwels. Et al. Fecal calprotectin is an early predictor of endoscopic response and histologic remission after the start of vedolizumab in inflammatory bowel disease. Therapeutic Advances in Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#组织学#
0
感谢分享
46
#内镜#
31
#预测指标#
29
#粪便#
24
#炎症性#
41
#炎症性肠病患者#
20
这是一项前瞻性研究。
83
#维多珠单抗#
112
#克罗恩病#
142